Results and Prognostic of pNO Laryngeal Cancer Treated by Post-Operative Irradiation
Mouden M, Semmar A, Rahali L, Kebdani T, Kacemi HI, Majjaoui S and Benjaafar N
DOI10.21767/2572-2107.1000014
Mouden M*, Semmar A, Rahali L, Kebdani T, Kacemi HI, Majjaoui S and Benjaafar N
Department of Radiotherapy, National Institute of Oncology, University Mohammed V, Rabat, Morocco
- *Corresponding Author:
- Mouden M
Radiation Oncologist
Department of Radiotherapy
National Institute of Oncology
University Mohammed V, Rabat, Morocco.
Tel: +212037563692
E-mail: moudenkarima@gmail.com
Received date: September 26, 2016; Accepted date: October 10, 2016; Published date: October 17, 2016
Citation: Mouden M, Semmar A, Rahali L, et al. Results and Prognostic of pNO Laryngeal Cancer Treated by Post-Operative Irradiation. Head Neck Cancer Res. 2016, 1:3. doi: 10.21767/2572-2107.100014
Introduction
Worldwide, there are approximately 130,000 new laryngeal cancer cases and 70,000 deaths annually. In the United States, laryngeal cancer accounts for about 25 percent of the 53,000 cases of head and neck cancer diagnosed annually [1]. Glottic, supraglottic, and subglottic cancers represent approximately two-thirds, one-third, and two percent of laryngeal cancers respectively. Survival rates of laryngeal cancer patients range from 73% to 92% for early disease stage (I and II) and from 50% to 64% for advanced stage (III and IV) [2]. Many prognostic factors have been studied and linked to the locoregional control and survival of laryngeal cancer. They include: resection margin, treatment modality, site of origin, disease stage, extracapsular spread, tumor volume, tumor grade, perineural invasion, lymphatic vessel density and nodal status [3-11].
The aim of our study is to investigate the survival and to determine prognostic factors of the larynx cancer in patients with pathological stage pN0.
Case Presentation
Between January 2011 and December 2012, a total of 102 patients were retrospectively analyzed. Subgroups of pN0 patients with laryngeal cancer included 38 patients. Primary surgical treatment consisted of total laryngectomy and neck dissection. The type of lymphadenectomy was selective neck dissection. The total dose of adjuvant radiotherapy was between 46 and 66 Gy in 2 Gy per fraction on the tumor bed. Concurrent chemotherapy with cisplatin 40 mg/m2/week was used in 5 cases which 4 with positive margins and one with close margin.
They were retrospectively analyzed. Local control rate, Overall survival (OS) and Disease-free survival (DFS) were calculated using SPSS 20. For the univariate analysis, we study prognostic variables: margin status, T stage and subglottic extension.
Results
Most of patients were males (97.4%). Median age was 58 years (range: 44-78). Subglottic extension was observed in 23 patients (60.5%). Stages I, II, III and IV patients accounted for 2.6%, 15.8%, 36.8% and 44.8% respectively. In this study, the median followup time was 29.5 months (6-58). In Table 1, the characteristics of the patients were summarized. The main characteristics were the predominance (81.5%) of advanced stage and the tumor extension.
| Characteristics | N (% or range) |
|---|---|
| Gender | |
| Male | 37 (97.4 %) |
| Female | 1 (2.6 %) |
| Age, Years (Median) | 58 (44-78) |
| Tobacco use | 31 (81.6%) |
| Alcohol use | 6 (15.8%) |
| Presenting symptom | |
| Neck mass | 0 |
| Hoarseness | 34 (89.5%) |
| Dysphagia | 6 (15.8%) |
| Dyspnea | 28 (73.7%) |
| Anatomic regions | |
| Supraglottis | 1 (2.7%) |
| Glottis | 5 (13.2%) |
| Subglottis | 2 (5.3%) |
| Supraglottis+Glottis | 9 (23.6%) |
| Subglottis+Glottis | 9 (23.6%) |
| Three anatomic regions | 12 (31.6%) |
| Pathologic type: Squamous cell carcinoma | 38 (100%) |
| T stage | |
| T1 | 1 (2.6%) |
| T2 | 6 (15.8%) |
| T3 | 14 (36.8%) |
| T4 | 17 (44.7%) |
| N stage | |
| N0 | 38 (100%) |
| M stage | |
| M0 | 38 (100%) |
| M1 | 0 |
| Surgery | |
| Larynx preservation surgery | 36 (94.7%) |
| Total laryngectomy | 2 (5.3%) |
| Positive margins | 4 (10.5%) |
| Close margins | 1 (2.6%) |
| Negative margins | 33 (86.8%) |
| Lymphovascular space invasion | |
| Yes | 1 (2.6%) |
| No | 37 (97.4%) |
| Perieural invasion | |
| Yes | 2 (5.3%) |
| No | 36 (94.7%) |
| Radiation therapy | |
| Postop chemo radiation therapy | 5 (13.1%) |
| Postop radiation therapy | 33 (86.9%) |
| Late toxicity | |
| Dysphagia | 2 (8.3%) |
| Xerostomia | 7 (28%) |
| Neck fibrosis | 5 (20.8%) |
Table 1: Patient characteristics.
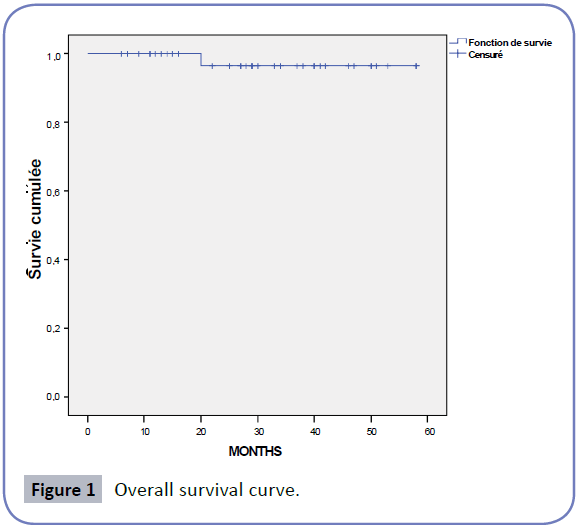
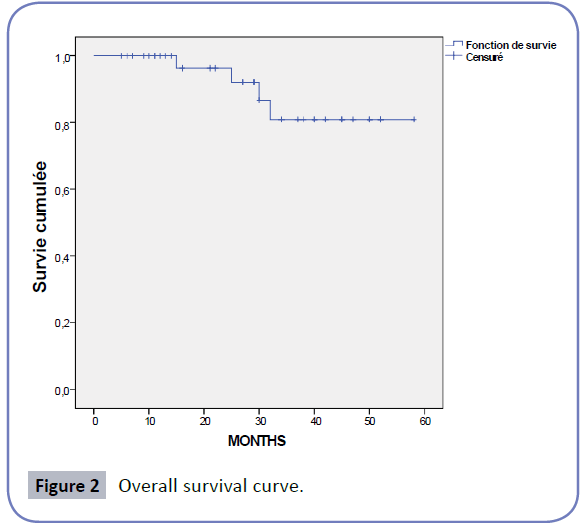
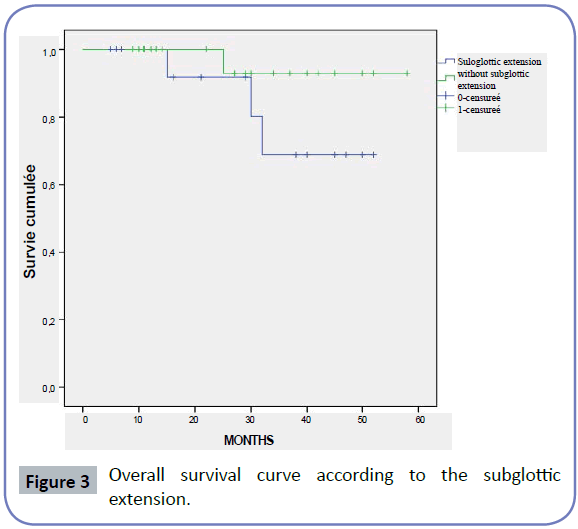
After a median follow-up of 29.5 months (6-58), we found one local relapse in the tumor bed which had positive margins, 3 distant relapses in the lung (7.9%) which had stage IV, and one death. No patient presented a nodal relapse. 2 patients (5.3%) were lost to follow-up. Local control rate was 89.5%. The 4- year overall survival (OS) and disease-free survival (DFS) rates were 96.4%, 80.9% respectively (Figures 1 and 2). The main long-term complications of therapy were xerostomia (28.9%), neck fibrosis (21%), dysphagia (7.8%) and hoarseness (16.7%). Univariate analysis demonstrated an insignificant influence on survival (p=0.21, p=0.50 and p=0.64) for subglottic extension, margin status, and T stage respectively) (Figure 3).
Discussion
Postoperative radiotherapy is generally restricted to patients thought to be at elevated risk of locoregional recurrence. It should be used with caution and only in those at risk because of the morbidity of postoperative radiotherapy and uncertainty regarding a survival benefit. Factors associated with an increased risk of locoregional recurrence after surgery include: Advanced tumor (T) stage (T3/T4), positive resection margins or tumor close to the resection margin, tumor extension through the lymph node capsule (extracapsular extension), two or more positive lymph nodes (N2/N3), perineural invasion and lymphovascular space invasion [12-20].
The prognosis of laryngeal carcinoma is related to a variety of clinical and histological factors, including nodal status. The presence of cervical positive lymph nodes is a significant predictor of poor survival outcomes in patients with laryngeal squamous cell carcinoma [9,21,22]. N stage decreases the disease-related survival by approximately 50% and is considered as the only significant factor for distant metastasis [6,9]. Published series node-negative cases were scarce. They were characterized by the extensively locally advanced tumor [23-25]. In our material, there was no significant effect of prognostic factors (margin status, T stage and subglottic extension) on the treatment results, but we found a good result for this sub group of pN0 laryngeal cancer (The local control rate, the 4-year overall survival (OS) and disease-free survival (DFS) rates were 89.5%, 96.4% and 80.9% respectively).
Clinical trials have demonstrated that postoperative concurrent chemoradiation therapy with cisplatin is more likely than postoperative radiation therapy (RT) alone to locoregional control disease and improve disease-free survival for patients with positive surgical margins and extracapsular extension [12,26,27].
Data supporting the use of postoperative RT without concurrent chemotherapy to improve locoregional control and survival is limited to two small randomized trials and retrospective observational data: One trial in 51 patients with advanced head and neck cancer found that the addition of RT to surgery decreased the overall recurrence rate [28]. However, no difference in overall survival was observed. A second trial, limited to 140 patients, all with squamous cell carcinoma of the oral cavity, did observe a statistically significant increase in disease-free survival at three years with postoperative RT compared to surgery alone [29]. In this study, the main cause of failure was distant metastases in the lung which were reported in 3 patients (7.9%). The main long-term complications of therapy were xerostomia (28%), neck fibrosis (20.8%) and dysphagia (8.3%).
According to the study by Nguyen-Tan et al. assessed a group of 223 laryngeal cancers postoperatively irradiated. They reported three tracheocutaneous fistula (1.3%) and three esophageal strictures (1.3%) [4].
Another study by Maillard et al. [30], including 166 patients with laryngeal cancer, fibrosis was noticed in 11 patients (7%) and tracheoesophageal fistula in two patients (1%).
The prognostic of larynx cancer stage N0, pN0 remains good. The main cause of failure was distant metastases in our study despite a small sample size.
Conclusion
Subgroups of patients with pathologically negative regional lymph nodes, despite the extensively locally advanced tumor, have a good local control and survival.
Declaration
KM, AS and LR were the major contributors in writing the manuscript. HE, TK, SM and NB cared for the patient during her time in the hospital and assisted in the data collection and the preparation of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
All authors are thankful for providing the necessary facilities for the preparation of the manuscript. Special thanks are due to the Faculty of Medicine and Pharmacy of Rabat, the source(s) of funding for all authors.
Availability of Data and Materials
The dataset supporting the conclusion of this article is presented in this manuscript.
Competing Interests
The authors declare that they have no competing interests.
Ethics, Approval and Consent
The research of this case report was conducted in accordance with the National Institute of Oncology of Rabat.
Funding
There were no financial support or relationships between the authors and any organization or professional bodies that could pose any conflict of interests.
References
- Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63: 11.
- Berrino F, De Angelis R, Sant M (2007) Survival for eight major cancers and all cancers combined for European adults diagnosed in 1995-99: results of the EUROCARE-4 study. Lancet Oncol 8: 733-783.
- Di Nicola V, Resta L, Rotundo L, Fiorella ML, Fiorella R (1999) Evaluation of resection margins as a prognostic factor in the surgical treatment of laryngeal carcinoma. Acta Otorhinolaryngol Italy 19: 325-341.
- Nguyen-Tan PF, Le QT, Quivey JM, Singer M, Terris DJ, et al. (2001) Treatment results and prognostic factors of advanced T3--4 laryngeal carcinoma: The University of California, San Francisco (UCSF) and Stanford University Hospital (SUH) experience. Int J Radiat Oncol Biol Phys 50: 1172-1180.
- Groome PA, Mackillop WJ, Rothwell DM, O’Sullivan B, Irish JC, et al. (2000) Management and outcome of glottic cancer: a population-based comparison between Ontario, Canada and the SEER areas of the United States. Surveillance, Epidemiology and End Results. J Otolaryngol 29: 67-77.
- Matsuo JMS, Patel SG, Singh B, Wong RJ, Boyle JO, et al. (2003) Clinical nodal stage is an independently significant predictor of distant failure in patients with squamous cell carcinoma of the larynx. Ann Surg 238: 412-421.
- Puri SK, Fan CY, Hanna E (2003) Significance of extracapsular lymph node metastases in patients with head and neck squamous cell carcinoma. Curr Opin Otolaryngol Head Neck Surg 11: 119-123.
- Strongin A, Yovino S, Taylor R, Wolf J, Cullen K, et al. (2012) Primary tumor volume is an important predictor of clinical outcomes among patients with locally advanced squamous cell cancer of the head and neck treated with definitive chemoradiotherapy. Int J Radiat Oncol Biol Phys 82: 1823-1830.
- Jose J, Coatesworth AP, MacLennan K (2003) Cervical metastases in upper aerodigestive tract squamous cell carcinoma: histopathologic analysis and reporting. Head Neck 25: 194-197.
- ChirilÃÆââ¬Å¾ÃâÃâ M, BolboacÃÆââ¬Å¾ÃâÃâ SD, Cosgarea M, Tomescu E, MureÃÆââ¬Â¦Ãâà ¸an M (2008) Perineural invasion of the major and minor nerves in laryngeal and hypopharyngeal cancer. Otolaryngol Head Neck Surg 140: 65-69.
- Audet N, Beasley NJ, MacMillan C, Jackson DG, Gullane PJ, et al. (2005) Lymphatic vessel density, nodal metastases, and prognosis in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 131: 1065-1070.
- Bernier J, Cooper JS (2005) Chemoradiation after surgery for high-risk head and neck cancer patients: how strong is the evidence? Oncologist 10: 215.
- Huang DT, Johnson CR, Schmidt-Ullrich R, Grimes M (1992) Postoperative radiotherapy in head and neck carcinoma with extracapsular lymph node extension and/or positive resection margins: a comparative study. Int J Radiat Oncol Biol Phys 23: 737.
- Ang KK, Trotti A, Brown BW (2001) Randomized trial addressing risk features and time factors of surgery plus radiotherapy in advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys 51: 571.
- Peters LJ, Goepfert H, Ang KK (1993) Evaluation of the dose for postoperative radiation therapy of head and neck cancer: first report of a prospective randomized trial. Int J Radiat Oncol Biol Phys 26: 3.
- Amdur RJ, Parsons JT, Mendenhall WM (1989) Postoperative irradiation for squamous cell carcinoma of the head and neck: an analysis of treatment results and complications. Int J Radiat Oncol Biol Phys 16: 25.
- Olsen KD, Caruso M, Foote RL (1994) Primary head and neck cancer. Histopathologic predictors of recurrence after neck dissection in patients with lymph node involvement. Arch Otolaryngol Head Neck Surg 120: 1370.
- Zelefsky MJ, Harrison LB, Fass DE (1993) Postoperative radiation therapy for squamous cell carcinomas of the oral cavity and oropharynx: impact of therapy on patients with positive surgical margins. Int J Radiat Oncol Biol Phys 25: 17.
- Jacobs JR, Ahmad K, Casiano R (1993) Implications of positive surgical margins. Laryngoscope 103: 64.
- Laramore GE, Scott CB, Schuller DE (1993) Is a surgical resection leaving positive margins of benefit to the patient with locally advanced squamous cell carcinoma of the head and neck: a comparative study using the intergroup study 0034 and the Radiation Therapy Oncology Group head and neck database. Int J Radiat Oncol Biol Phys 27: 1011.
- Zhang SY, Lu ZM, Luo XN (2013) Retrospective analysis of prognostic factors in 205 patients with laryngeal squamous cell carcinoma who underwent surgical treatment. PLoS One 8: e60157.
- Zhao H, Ren J, Zhuo X, Ye H, Zou J, et al. (2008) Prognostic significance of survivin and CD44v6 in laryngeal cancer surgical margins. J Cancer Res Clin Oncol 134: 1051-1058.
- Layland MK, Sessions GE, Lenox J (2005) The influence of lymph node metastases in the treatment of squamous cell carcinoma of the oral cavity, oropharynx, larynx and hypopharynx: N0 versus N+. Laryngoscope 115: 629-639.
- Sas-KorczyÃÆââ¬Â¦Ãâââ¬Å¾ska B (1998) Analysis of causes of treatment failure in patients with advanced laryngeal cancer treated with total laryngectomy and postoperative irradiation. Nowotwory 48: 643-662.
- Wieczorek A, Fijuth J, Michalski W (2002) The results of postoperative irradiation for locally advanced carcinoma of the larynx. Nowotwory 52: 287-294.
- Cooper JS, Pajak TF, Forastiere AA (2004) Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med 350: 1937-1944.
- Cooper JS, Zhang Q, Pajak TF (2012) Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 84: 1198.
- Kokal WA, Neifeld JP, Eisert D (1988) Postoperative radiation as adjuvant treatment for carcinoma of the oral cavity, larynx, and pharynx: preliminary report of a prospective randomized trial. J Surg Oncol 38: 71.
- Mishra RC, Singh DN, Mishra TK (1996) Post-operative radiotherapy in carcinoma of buccal mucosa, a prospective randomized trial. Eur J Surg Oncol 22: 502.
- Maillard S, Jovenin M, Cauchois A, Froissart D, Merol JC, et al. (2005) Radiothérapie postopératoire des cancers larynges classes N0. Cancer Radiothér 9: 285-292.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences