Diagnostic Paradox behind Facial Nerve Schwannoma
Saumya Mishra, Haritosh K Velankar, Merin Sara Mathew, Roshni K and Yogesh G Dabholkar
DOI10.21767/2572-2107.100020
Saumya Mishra*, Haritosh K Velankar, Merin Sara Mathew, Roshni K and Yogesh G Dabholkar
Department of ENT, DY Patil Hospital and Research Centre, Navi Mumbai, India
- *Corresponding Author:
- Mishra S
Department of ENT, DY Patil Hospital
and Research Centre, Navi Mumbai, India
Tel: +91-9552763306
E-mail: msaumya18@gmail.com
Received Date: 17 November 2017 Accepted Date: 27 November 2017 Published Date: 04 December 2017
Citation: Mishra S, Velankar HK, Sara M, Roshni M, Yogesh K, et al. Diagnostic Paradox behind Facial Nerve Schwannoma. Head Neck Cancer Res. 2017, Vol.2 No.2:5. DOI: 10.21767/2572-2107.100020
Copyright: © 2017 Mishra S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Schwannomas are benign and slow growing tumors that arise from the Schwann cells which ensheath the axons of peripheral nerve, cranial nerve and autonomic nervous system. A schwannoma of facial nerve may originate from extra or intra cranial segments of the nerve. Most of the facial nerve schwannomas originate from intra-tympanic region. In decreasing order of their frequency, schwannomas were found along the tympanic, mastoid (vertical), labrynthine and meatal segments of the facial nerve. It is an extremely rare entity as malignant degeneration of schwannomas is not frequent. A high level of clinical suspicion with detailed neuro-otological and radiological studies play important role in preoperative diagnosis of schwannomas.
Case presentation: We reported a case of 35-year-old male with progressive right sided facial asymmetry, sudden onset hearing loss and non-pulsatile tinnitus in right ear. The patient’s presentation and diagnostic examinations helped us to reach a provisional diagnosis though final diagnosis was done on the basis of histopathological examination of the excised tumor which was suggestive of facial nerve schwannoma.
Conclusion: The rare and inconsistent clinical presentation and radiological pattern of facial schwannoma often leads to a delayed and indefinite diagnosis. The critical step in management of diverse lesion is diagnosis for the management of facial schwannoma. This report is about a challenging case of facial nerve schwannoma in intra-tympanic region which was diagnosed and managed in our institution.
Keywords
Facial nerve schwannoma; Facial palsy; Shwannoma
Introduction
Virchow first reported schwannoma in 1908, a tumor arising from the neural sheath of the peripheral sensory, motor, sympathetic, and cranial nerves.
Schwannoma is an ectodermal, benign, encapsulated and solitary tumor that originates from Schwann cells of peripheral nerve sheath [1]. They have a tendency to push axons of nerve of origin away [2] and so that they can potentially be resected with nerve preservation. They occasionally feature areas of calcification or cystic degeneration. Neurogenic neoplasms of facial nerve are uncommon [1]. Facial nerve schwannoma are rare and benign intra-tympanic tumors arising from any segment of nerve with a special predilection for the geniculate area which is most commonly involved [3,4]. The nerve of origin can be identified macroscopically or microscopically. In the macroscopic appearance, tumor is found attached to the nerve and is firm to rubbery in consistency with tan-white to yellow color [5]. Sometimes the tumor is mistaken as a lymph node and is excised without seeking to preserve or repair the nerve. Facial nerve is made up of numerous fascicles each containing a bundle of nerve fibers bounded by connective tissue. A small amount of connective tissue is arranged around and through the fascicles forming a delicate sheath over its surface because of this structure [6], iatrogenic nerve injury is increased during surgery. The intra-cranial portion of facial nerve is devoid of epineurium [7]. Lack of epineurium leads to effacement of facial nerve and spreading of individual fascicles over the surface of large facial schwannoma. Between the lateral end of internal auditory meatus and branch to stapedius, the fascicles of facial nerve form single bundle [6]. Distal to the branch to stapedius, the single bundle divides to form multiple fascicles each with a well-defined perineurium within the surrounding epineurium [6].
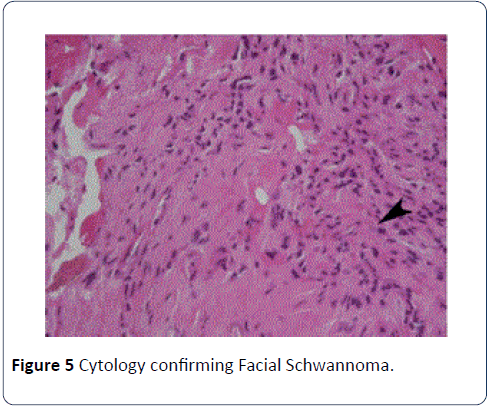
Histologically, Antoni-A areas consist of the distinctive short fascicles of palisaded Schwann cells with wavy nuclei make up in the cellular areas and diagnostic verocay bodies, and the intervening paucicellular zones are myxoid in Antoni-B area [5]. Symptoms most often include dysfunction of seventh or eighth cranial nerve accompanied with hearing loss, tinnitus and dizziness. Their clinical presentation is variable ranging from complete facial palsy to sometimes even normal facial nerve function.
Multiple radiological patterns have been reported but none of them are pathognomonic. In Computerized Tomography and Magnetic Resonance Imaging, the mass appears identical to vestibular schwannoma and key to diagnosis is neuroanatomic location of tumor [8-11]. Magnetic Resonance Imaging makes it easy to identify the internal structure by outlining all the soft tissues and providing specific information regarding tumor. For patients with mild or no facial dysfunction, a conservative attitude with observation is preferred. The surgical approach depends upon tumor extension and location. One of the major risk is damage to facial nerve resulting in weakness or paralysis of affected side of face mostly seen in intra-tympanic region. If facial nerve has been preserved then there are chances of safeguarding facial function, but not completely. In extreme cases facial nerve has to be sacrificed, thus a permanent facial paralysis is inevitable.
Case report
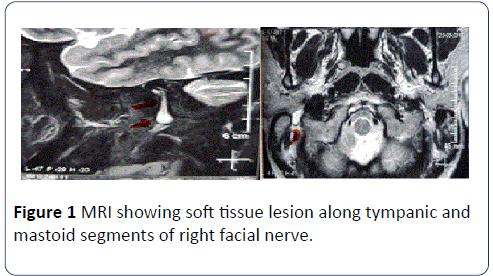
A 35-year-old man presented to our hospital with complaints of progressive right facial weakness and intermittent twitching of the right eyelid accompanied by hearing loss, tinnitus and sensation of fullness in right ear for 1 month. He had no previous history of facial nerve surgery or head trauma. However physical examination revealed grade-2 facial palsy on right side. On examination under microscope of the right ear, a whitish mass was found in posterior-inferior quadrant with grade-2 retraction of right tympanic membrane. Preoperative magnetic resonance imaging (MRI) showed soft tissue lesion along tympanic and mastoid segments of right facial nerve, widening bony canal and bulging out through stylo-mastoid foramen (Figure 1).
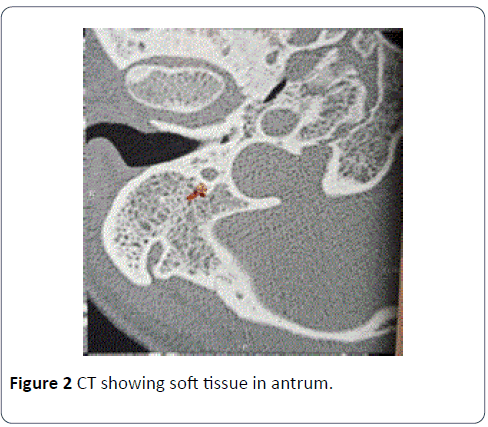
Computerized tomography imaging revealed soft tissue in antrum, widening of bony canal throughout temporal bone beyond anterior genu with small soft tissue in right mesotympanum, resorption of lateral wall of cochlea, stapes suprastructure and long process of incus (Figure 2).
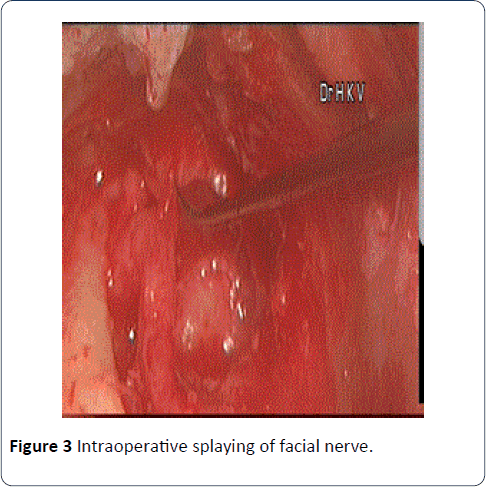
The patient was preoperatively counselled about the possible chances of no improvement in facial palsy or even worsening of the same. Resection of tumor with preservation of facial nerve function was the surgical challenge. Intraoperatively, tumor was splayed around its capsule which was closely adherent to nerve trunk and providing compression over the nerve (Figure 3).
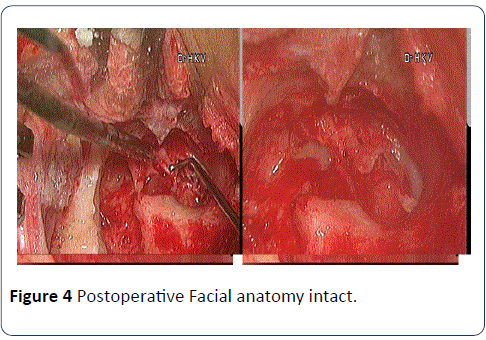
As can be seen it was located in the intra-tympanic region extending from first genu of the facial nerve up to stylomastoid foramen. Surgical excision of complete tumor was achieved by separation of healthy fascicles and removal of fascicles from which tumor originates and then the tumor was stripped from nerve surface leaving the nerve anatomy intact (Figure 4).
Facial nerve decompression was done, and excised specimen was sent for histopathology. We observed a great degree of difficulty while resection of tumor due to its intimate involvement with facial nerve. On histopathology, tumor cells showed hypo-cellular and hyper-cellular areas. Hyper-cellular areas (Antoni A) are composed of spindle shaped cells arranged in interlacing fascicles having a comma shaped nucleus with pointed ends and scanty cytoplasm. Hypo-cellular areas (Antoni B) are made up of oval cells which are haphazardly arranged in a fibrillary myxoid background (Figure 5) confirming the diagnosis of facial schwannoma.
In the post-operative follow up after three months patient showed significant improvement in facial palsy with the help of physiotherapy.
Discussion
Facial nerve schwannomas are rare and slow growing tumor which account for less than 1% of all temporal bone tumors that tend to occur during middle age with male predominance [1,12]. They are typically solitary, unilateral and sporadic in nature. Sometimes facial nerve schwannoma is bilateral as part of neurofibromatosis-2 spectrum. The facial nerve schwannoma usually manifest with facial palsy and often with an insidious onset. Normal facial function has been reported in 27 to 54% of cases but a small and significant percentage of patients demonstrate some degree of facial dysfunction when evaluated by careful exploration. Hearing loss and tinnitus are common among patients with facial nerve schwannomas. A literature review indicates that less than 50% of the facial nerve can be completely preserved during surgery [12,13]. The treatment decision should be tailored according to tumor growth, hearing function, surgical experience and facial function deterioration. For those patients going for surgery, surgeon has to counsel adequately the patients and prepare them for the possibility of facial nerve sacrifice, and discuss other rehabilitation options such as nerve graft [14].
Vestibular schwannoma also known as acoustic neuroma is a rare slow growing tumor arising from vestibular-cochlear nerve. Due to its resemblance to facial schwannoma, diagnosis can be resolved by detailed imaging which determines the location and size of tumor. These pathoanatomic facts about facial schwannoma complicate any attempt to treat this tumor and also alter the benefits of treatment before developing serious complications.
FNSs show multi-segmental involvement which acquires a dumbbell shape, narrow labrynthine segment forms the isthmus of dumbbell between the globular tumor component at Internal acoustic canal and geniculate ganglion. Occasionally, the geniculate ganglion component of a dumbbell shaped FNS erodes into cochlea and thus mimics a transmodiolar acoustic schwannoma.
Geniculate ganglion fossa is considered as the most common site for occurrence of FNS with its extension till tympanic or labyrinthine segments. This location is also a common site for occurrence of facial nerve hemangiomas. In about 50% cases, facial nerve hemangiomas may not show their characteristic honeycomb or internal bony spicules on CT. However, FN hemangiomas present poorly defined margins on HRCT which differentiate them from FNSs with smooth margins.
Schwannomas and Neuro-fibromas are nerve damaging masses. Neuro-fibromas are classified as diffuse or plexiform which are typically non- encapsulated. They are intimately associated with the nerve, making resection with nerve preservation difficult. Unlike schwannoma, malignant preservation difficult. Unlike schwannoma, malignant degeneration has been reported in neuro-fibromas.
A facial nerve schwannoma in parotid is rarely seen [15,16]. Schwannoma should be suspected if facial nerve cannot be found intraoperatively or if the intra-tympanic tumor is associated with the facial nerve. Facial nerve paralysis associated with parotid tumor suggests malignancy and the neural dysfunction due to schwannoma is attributed due to compressive effect of tumor. The parotid mass is always painless and gradually increases in size, extra temporally they are present as asymptomatic parotid mass [2,17].
CT imaging provides useful information for preoperative planning, but MRI is the method of choice for evaluating facial nerve schwannomas.
The treatment of facial nerve schwannomas consists of removing tumor from the involved facial nerve segment and restoring facial function with a cable graft or a nerve crossover graft depending upon the size and location of tumor. The optimal timing of treatment for facial nerve schwannomas is also controversial. Because postoperative facial function is usually poor in these patients, some authors advocate a policy of close follow up with serial MRI. Surgery would be indicated when facial paralysis progresses or when significant compression of vital structures is noted.
Given the potential for injury of the facial nerve, the surgeon must have a clear management algorithm if facial nerve is encountered. Because the outcome of a biopsy or partial resection on postoperative facial function may be unpredictable, intraoperative decisions should be individualized.
Conclusion
Facial nerve schwannomas are relatively uncommon but when present are mostly seen in intra-tympanic region. Facial dysfunction along with tinnitus and hearing loss may alert clinician to the possibility of a facial nerve tumor. However, in absence of obvious facial nerve dysfunction the diagnosis may be missed. Facial nerve schwannomas have variable patterns of clinical presentations and therefore the diagnosis is often not known preoperatively. Only a high index of suspicion and awareness of this probable diagnosis will prompt a thorough radiological examination essential to clinch the diagnosis. It appears that the clinical presentation is helpful only if there is a history of slow gradual facial paresis associated with a slow growing tumor.
References
- Monagle B, Al- Sanosi A, Croxson G, Fagan P (2008) Facial schwannoma; results of a large case series and review. J Laryngol Otol 122: 1139-1150.
- Kumar BN, Walsh RM, Walter NM (1996) Intraparotid facial nerve schwannoma in child. J Laryngol Otol 110: 1169-1170.
- Storper IS, Glasscock ME III, Jackson CG, Ishiyama A, Bruce JN (1998) Management of nonacoustic cranial nerve neuromata. Am J Otol 19: 484-490.
- Doyle KJ, Amin N, Peck WW (1997) Imaging case of the month:facial nerve neuroma. Am J Otol 18: 518-519.
- Ram Moorthy, Adrian T Warfield (2013) Head and neck pathology. Stell and Maran, 5th edn. p: 93.
- Van Buskirk C (1945) The seventh nerve complex. Journal of Comparative Neurology 82: 303-335.
- Sunderland S, Cossar DF (1953) The structure of facial nerve. Anatomical Record 116: 147-162.
- Moffat DA, Ballagh RH (1995) Rare tumours of the cerebellopontine angle. Clinical Oncology (Royal College of Radiologists (Great Britain)) 7: 28-41.
- Bonneville F, Sarrazin JL, Marsot-Dupuch K, Iffenecker C, Cordoliani YS, et al. (2001) Unusual lesions of the cerebellopontine angle: A segmental approach. Radiographics 21: 419-438.
- Lalwani AK (1992) Meningiomas, epidermoids and other nonacoustic tumours of cerebellopontine angle. Otolaryngologic Clinics of North America 25: 707-728.
- Bartels LJ, Arrington JR (1994) Rare tumours of the cerebellopontine angle. In: Jackler RK, Brackmann D (eds.), pp: 835-861.
- Perez R, Chen JM, Nedzelski JM (2005) Intratemporal facial nerve schwannoma; a management dilemma. Otol Neurotol 26: 121-126.
- Falcioni M, Russo A, Taibah A, Sanna M (2003) Facial nerve tumour. Otol Neurotol 24: 942-947.
- Shirazi M, Leonetti JP, Marzo SJ, Anderson DE (2007) Surgical management of facial neuromas; lessons learned. Otol Neurotol 28: 958-963.
- Mc Guirt WF, Johnson PE, Mc Guirt WT (1987) Intraparotid facial nerve neurofibromas. Laryngoscope 97: 219-223.
- Saeed SR, Wool TJ, Ramsden RT, Lye TH (1995) Magnetic resonance imaging; a cost effective first line investigation in the detection of vestibular schwannoma. BJ Neurosurgery 9: 315-321.
- Shaha AR, Weber C, DiMaio T, Jaffe BM (1990) Needle aspiration biopsy in salivary gland lesions. Am J Surg 160: 373-376.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences