Effectiveness of Chemoradiotherapy for T1b-T2 Glottic Carcinoma
Kubo K and Kiriu H
DOI10.21767/2572-2107.100011
Kubo K and Kiriu H*
Department of Radiation Oncology, Hiroshima City Asa Citizens Hospital, 2-1- 1 Kabeminami Asakitaku Hiroshima-shi, Hiroshima, Japan
- *Corresponding Author:
- Kiriu H
Department of Radiation Oncology
Hiroshima City Asa Citizens Hospital
2-1- 1 Kabeminami Asakitaku Hiroshima-shi
Hiroshima, Japan
Tel: 082-815-5211
E-mail: hhkiriu@rd6.so-net.ne.jp (or) maro1987@hotmail.co.jp
Received date: June 21, 2016; Accepted date: July 17, 2016; Published date: July 25, 2016
Citation: Kubo K, Kiriu H. Effectiveness of Chemoradiotherapy for T1b-T2 Glottic Carcinoma. Head Neck Cancer Res. 2016, 1:2.
Abstract
Local control rates for T1b-T2 glottic carcinoma are not satisfactory. The purpose of this study was to evaluate the outcomes of patients with T1-T2 glottic carcinoma treated with radiotherapy and to evaluate the effects of chemoradiotherapy for T1b and T2 disease. At Hiroshima City Asa Citizens Hospital, 49 patients with early glottic carcinoma underwent radiotherapy from July 2006 to December 2015. Of these, 46 patients were enrolled and evaluated. The median age was 70.5 years (range, 39-88 years), and 43 patients (93.5%) were men and 3 patients (6.5%) were women. All patients presented with squamous cell carcinoma. Twenty-eight (60.1%) had T1a, 6 (13%) had T1b and 12 (26.1%) had T2 disease. In T1 and T2 patients, 2 Gy/fraction was used and the total prescribed dose ranged from 60 to 66 Gy and from 60 to 70 Gy, respectively. The patients with T1b and T2 were administered chemotherapy. The patients with T1 disease had a 5-year local control rate of 90.9%, while patients with T2 disease had a local control rate of 80.0%. The patients with T1a disease had a 5-year local control rate of 88.9%, while patients with T1b disease had a local control rate of 100%. Chemoradiotherapy for patients with T1b-T2 glottic carcinoma is feasible and may contribute to improved local control of patients with T1b disease.
Keywords
Glottic carcinoma; Radiotherapy; Chemoradiotherapy; Local control
Introduction
Glottic cancer is the most common laryngeal cancer. Patients with T1-T2N0 squamous cell carcinoma of the glottic larynx may be treated with transoral laser excision, open partial laryngectomy, or radiotherapy [1]. Radiotherapy for early glottic carcinoma results in good clinical outcome and can preserve the structure and function of the larynx. Many studies showing the effectiveness of radiotherapy for glottic carcinoma have been reported. It is important to continue to confirm the effectiveness of this treatment in the future.
For T1 glottic carcinoma, the 5-year local control rate has been reported to be approximately 80-90%, whereas for T2 glottic carcinoma, the local control rate is 70-80% [1-6]. In T1 disease, T1b glottic carcinoma tends to have a lower local control rate of approximately 80% [2-4]. These results are not satisfactory, especially for T2 cases. If local recurrence is observed in patients who were initially treated with radiotherapy, the patients will undergo salvage surgery. This results in poorer voice quality. Therefore, it is very important to control the primary tumor lesion. Several studies have reported that chemoradiation was safe and effective for T2 glottic carcinoma [7-10]. However, there are few published studies that evaluated the effects of chemoradiation for T1b disease.
The purpose of this study was to evaluate the outcomes of patients with T1-T2 glottic carcinoma treated with radiotherapy and to evaluate the effects of chemoradiotherapy for T1b and T2 disease.
Methods
Patient eligibility
After At Hiroshima City Asa Citizens Hospital, 49 patients with early glottic carcinoma underwent radiotherapy from July 2006 to December 2015. Eligibility criteria included T1 or T2 disease, age over 20 years, Eastern Cooperative Oncology Group performance status of 0-2, a histologic diagnosis of infiltrative squamous cell carcinoma and no previous radiation therapy (RT) for head and neck neoplasms.
Before therapy, all patients were evaluated clinically with a medical history, physical examination, laboratory examination, computed tomography (CT) scan of the whole body, and upper endoscopy. The laboratory examination included a complete blood cell count, liver function studies, renal function studies, and measurement of electrolytes. Smoking status was expressed by the Brinkman index, which is calculated as the number of cigarettes per day multiplied by years of smoking.
Treatment procedure for radiotherapy
Three-dimensional (3D) conformal radiation therapy was used for all patients. For 3D treatment planning, CT scanning (Light Speed RT; GE, Milwaukee, Wisconsin) was performed under freebreathing conditions. CT volume data were transferred to a 3D treatment planning system (Xio; ELEKTA, Stockholm, Sweden). Forty-six patients were treated with non-parallel opposed fields using 6-MV photons from the linear accelerator.
In T1 patients, 2 Gy/fraction was used and the total prescribed dose ranged from 60 to 66 Gy (median 60 Gy). In T2 patients, 2 Gy/ fraction was used and the total prescribed dose ranged from 60 to 70 Gy (median 60 Gy). Wedge filters of 15 or 30 degrees were used to optimize the dose distribution to achieve a homogeneity of ± 5%. No prophylactic neck irradiation was performed in any of the cases. All patients were immobilized using a thermoplastic mask during treatment.
Chemotherapy
Eighteen patients (39.1%) were administered chemotherapy. The patients with T1b and T2 carcinoma were administered chemotherapy. The basic regimen was weekly carboplatin (CBDCA, area under the curve [AUC], 1.5-2.0), and 9 patients received this regimen concurrently with RT. Two patients received cisplatin plus 5-fluorouracil concurrently with RT. Seven patients received S-1. Two patients with T1b disease did not undergo chemotherapy because of the presence of various comorbidities.
Evaluation
Tumor response and recurrence were analyzed by the findings of fiberscopes by the otolaryngologist. We also evaluated adverse effects, especially radiation dermatitis and mucositis, using Common Terminology Criteria for Adverse Events (CTCAE) version 4.0.
Follow-up
Patients were followed at regular intervals, usually every month for the first year after treatment, every 2 months for 2 years, every 3 months after 3-4 years and then every 4 months after 5 years if the patient had no evidence of recurrence. The follow-up evaluation routinely included a physical examination, fiberscopes, neck ultrasonography, and blood tests.
Statistical methods
Univariate analyses using the Mantel-Haenszel χ² test were performed to determine the statistical significance of differences in responses. The Kaplan-Meier method was used to calculate the local control rates. Statistical significance was defined as P<0.05.
Results
Patient characteristics
Forty-nine patients with T1-T2 carcinoma underwent RT from July 2006 to December 2015. Among them, 46 patients were enrolled and evaluated. Three patients were excluded; one patient was changing hospitals immediately after the treatment and two patients stopped coming to the hospital during or after treatment.
The patients’ clinical characteristics are summarized in Table 1. The median age was 70.5 years (range, 39-88 years), and 43 patients (93.5%) were men and 3 patients (6.5%) were women. All patients presented with squamous cell carcinoma. Twenty-eight (60.1%) had T1a, 6 (13%) had T1b and 12 (26.1%) had T2 disease. Details of their chemotherapy are shown in Table 2.
| Gender | percentage | |
|---|---|---|
| Male | 43 | 93.5 |
| female | 3 | 6.5 |
| Age (median) | 39-88 (70.5) | |
| Performance status (ECOG) | ||
| 0-1 | 46 | 100 |
| 2 | 0 | 0 |
| Histology | ||
| Squamous cell carcinoma T factor | 46 | 100 |
| 28 | 60.9 | |
| 1b | 6 | 13 |
| 2 | 12 | 26.1 |
Table 1: Clinical characteristics of glottic cancer patients.
| T1a patients | |
|---|---|
| weekly CBDCA | 1 patient |
| TS-1 | 1 patient |
| none | 26 patients |
| T1b patients | |
| weekly CBDCA | 3 patients |
| TS-1 | 1 patient |
| none | 2 patients |
| T2 patients | |
| weekly CBDCA | 5 patients |
| CDDP + 5-FU | 2 patients |
| TS-1 | 5 patients |
Table 2: Details of chemotherapy.
Local control rate and the pattern of failure
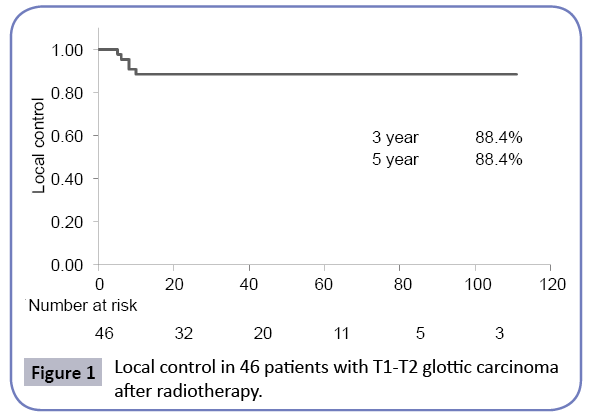
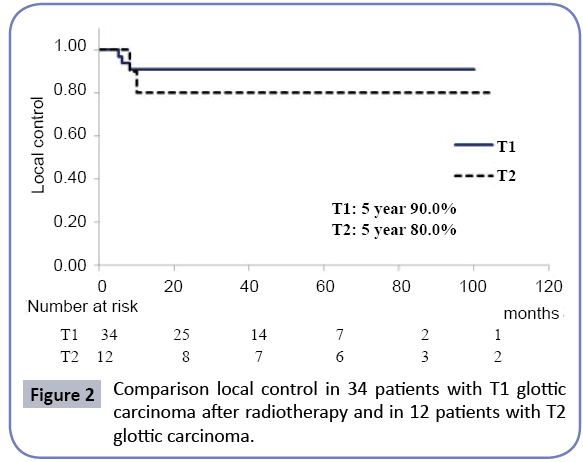
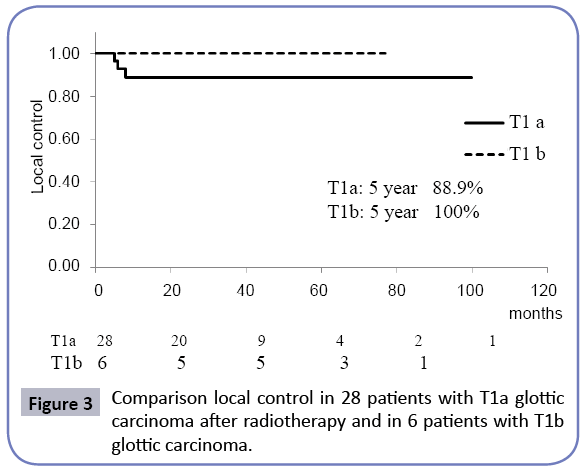
For all 46 patients, the 3 and 5-year local control rates were 88.4% (Figure 1). Patients with T1 disease had 3 and 5-year local control rates of 90.9%, while patients with T2 disease had 3 and 5-year local control rates of 80.0% (Figure 2). The patients with T1a disease had a 5-year local control rate of 88.9%, while patients with T1b disease had a local control rate of 100% (Figure 3). In patients who had T1b disease, none had local recurrence.
Of the 46 patients, disease recurrence was recorded in 6 patients. Local recurrences occurred in 5 patients (10.9%), and these 5 patients underwent salvage surgery. One patient had lymph node recurrences in the neck. In the final analysis, only one patient who had T2 disease died of glottic carcinoma.
Overall survival and cause-specific survival
The 3 and 5-year overall survival rates for all patients were 97.4%. The 5-year overall survival rates for T1a, T1b, and T2 were 100%, 100%, and 88.9% respectively. The 3 and 5-year cause-specific survival rates for all patients were 97.4% and 97.4%, respectively. The 5-year cause-specific survival rates for T1a, T1b, and T2 were 100%, 100%, and 88.9% respectively.
Univariate analysis
The variables analyzed in 46 patients included age, T factor, described dose, chemotherapy and Brinkman index for local control (Table 3). Age (<75 years) was a significant predictive factor of the local control rate in the univariate analysis (P=0.0463). Although no significant differences were identified, a Brinkman index of ≥ 800 tended to lead to inferior local control (P=0.0579).
| Prognostic factor | 5-year LC (%) | UVA*P | |
|---|---|---|---|
| Age, years | <75 | 96.2 | 0.0463 |
| ≥75 | 76.5 | ||
| T factor | T1 | 90.9 | 0.405 |
| T2 | 80 | ||
| Radiotherapy | 60 Gy | 85.2 | 0.376 |
| >60 Gy | 93.8 | ||
| Chemotherapy | None | 88.9 | 0.95 |
| combined | 87.5 | ||
| Brinkman index** | <800 | 100 | 0.0579 |
| ≥800 | 80.8 | ||
Table 3: Prognostic factor; univariate analysis.
Treatment-related toxicities
Grade 1 radiation mucositis was detected in 10 patients (21.7%), grade 2 in 28 patients (60.9%), and grade 3 in 3 patients (6.5%). Grade 1 radiation dermatitis was detected in 32 patients (69.6%), grade 2 in 8 patients (17.4%), and grade 3 in 1 patient (2.8%).
Second primary cancers
Seventeen patients (37.0%) had second primary cancers, and 3 patients (6.5%) had third primary cancers. The sites of second and third primary cancers are shown in Table 4. In the 20 primary lesions, 13 lesions (65%) were in the aerodigestive tract.
| Primary site | Number | Percentage |
|---|---|---|
| Esophagus | 1 | 5 |
| Stomach | 4 | 20 |
| Lung | 4 | 20 |
| Colon | 4 | 20 |
| Pancreatic | 1 | 5 |
| Bladder | 1 | 5 |
| Prostate | 3 | 15 |
| Others | 2 | 10 |
| Total | 20 | 100 |
| *UVA: univariate analyses **Brinkman index is calculated as the number of cigarettes per day multiplied by years of smoking. |
||
Table 4: Incidence of secondary primary cancers in this study.
Discussion
Radiotherapy for early glottic carcinoma shows good clinical outcome. Table 5 lists the results of radiotherapy studies for early glottic carcinoma. Several studies reported that the 5-year local control rates of T1 disease were approximately 80-90% [11]. In our study, patients with T1 disease had 3 and 5-year local control rates of 90.9%. When compared to other reports, this result is not inferior.
| Author (Year) | T factor | No. of patients | Prescribed dose | Local control rate |
|---|---|---|---|---|
| Nishimura | T1 | 96 | 60-66Gy | 85% |
| -1996 | T2 | 32 | 71% | |
| Burke | T1a | 68 | 65Gy | 92% |
| -1997 | T1b | 7 | 80% | |
| T2a* | 18 | 94% | ||
| T2b* | 9 | 23% | ||
| Warde | T1a | 403 | 50Gy | 91% |
| -1998 | T1b | 46 | 82% | |
| T2 | 286 | 69% | ||
| Onimaru | T1a | 146 | 65Gy | 89.80% |
| -2011 | T1b | 54 | ||
| Harada | T1a | 54 | 66Gy | 92% |
| -2015 | T1b | 26 | 70Gy | 83% |
| T2 | 35 | 74.4Gy | 86% | |
| This study | T1a | 28 | 60Gy | 88.90% |
| -2016 | T1b | 6 | 100% | |
| T2 | 12 | 80% |
Table 5: Summary of radiation therapy for early glottic carcinoma.
In T1 disease, the T1b glottic carcinoma local control rate, approximately 80%, tends to be lower than it is in T1a disease [2-4]. These results are not satisfactory. However, at present, the standard evidence-based treatment for T1b glottic carcinoma is radiotherapy, not chemoradiotherapy [12]. Several studies reported the results of glottic carcinoma treated with chemoradiotherapy to control the primary tumor lesion; Hirasawa et al. [9] reported that the 5-year local control rate was 83%. In those studies, treatment consisted of radiotherapy in fractions of 2 Gy for a median total dose of 70 Gy, and 30% of the patients with T1b disease were given chemotherapy. In the study reported here, patients with T1b disease were administered chemotherapy concurrently, and had a 5-year local control rate of 100%.
For T2 glottic carcinoma, the 5-year local control rate is 70- 80%. Several studies reported that chemoradiation was safe and effective for T2 glottic carcinoma [7-9,13]. Niibe et al. [8] reported that the 5-year local control rate was 83.4%. In that study, treatment consisted of radiotherapy in fractions of 2 Gy for a total dose of 60 Gy, and the patients received chemotherapy concurrently. Akimoto et al. [10] demonstrated that concurrent chemoradiotherapy of T2N0 laryngeal carcinoma produced a better local control rate than conventional radiotherapy alone and reported that the 5-year local control rate was 89%. The chemoradiotherapy method used was a combination of radiotherapy and intravenous chemotherapy. In our study, patients with T2 disease had a 3-year local control rate of 80.0% and a 5-year local control rate of 80.0%, respectively. The results of this study, when compared with previous results, are not inferior.
Various prognostic factors influencing local control were reported. Santhi et al. [11] reported that recurrence of laryngeal cancer was associated with continued smoking which was significant in univariate analysis. Tobacco smoking is the most important etiological factor. Several studies reported that tobacco smoking during radiation therapy for head-and-neck cancer was associated with poor outcomes [14,15]. In our study, no patient who smoked during radiotherapy was observed; therefore, we focused on past history of smoking. Although no significant differences were identified, a Brinkman index ≥ 800 was associated with inferior local control (P=0.0579). In addition, age (<75 years) was a significant predictive factor of the local control rate in the univariate analysis (P=0.0463).
Conclusion
In our study, patients with T1 disease had a 5-year local control rate of 90.9%, while patients with T2 disease had a local control rate of 80.0%. The patients with T1b disease had a 5-year local control rate of 100%. Chemoradiotherapy for patients with T1b-T2 glottic carcinoma is feasible and may contribute to improved local control in patients with T1b glottic carcinoma.
Funding
This research was carried out without funding.
Competing and Conflicting Interests
No author has any competing and conflicting interests.
References
- Johnson JT, Mendenhall WM, Werning JW, Hinerman RW, Amdur RJ, et al. (2004) Management of T1-T2 glottic carcinomas cancer. Cancer 100: 1786-1792.
- Burke LS, Greven KM, McGuirt WT, Case D, Hoen HM, et al. (1997) Definitive radiotherapy for early glottic carcinoma: Prognostic factors and implications for treatment. IntJ Radiat Oncol Biol Phys 38: 1001-1006.
- Warde PO, Sullivan B, Bristow RG, Panzarella T, Keane TJ, et al. (1998) T1/T2 Glottic cancer managed by external beam radiotherapy: the influence of pretreatment hemoglobin on local control.IntJ Radiat Oncol Biol Phys 41: 347-353.
- Harada A, Sakai R, Miyawaki D, Yoshida K, Nishimura K, et al. (2015) Treatment outcomes of the patients with early glottic cancer treated with initial radiotherapy and salvaged by conservative surgery. Jpn J Clin Oncol 45: 248-255.
- Nishimura Y, Nagata Y, Okajima K, Mitsumori M, Hiraoka M, et al. (1996) Radiation therapy for T1, 2glottic carcinoma: impact of overall treatment time on local control. Radiother Oncol 40: 225-232.
- Onimaru R, Hasegawa M, Yasuda K, Homma A, Oridate N, et al. (2011) Radiotherapy for glottic T1N0 carcinoma with slight hypofractionation and standard overall treatment time: importance of overall treatment time. Jpn J Clin Oncol 41: 103-109.
- Nakayama M, Hayakawa K, Okamoto M, Niibe Y, Ishiyama H, et al. (2010) Phase I/II trial of concurrent use of S-1 and radiation therapy for T2 glottic cancer.Jpn J Clin Oncol 40: 921-926.
- Niibe Y, Nakayama M, Matsubayashi T, Takahashi H, Kitano M, et al. (2007) Effectiveness of concurrent radiation therapy with UFT or TS-1 for T2N0 glottic cancer in japan. Anticancer Res 27: 3497-3500.
- Hirasawa N, Itoh Y, Ishihara S, Kubota S, Itoh J, et al. (2010) Radiotherapy with or without chemotherapy for patients with T1-T2 glottic carcinoma: retrospective analysis. Head Neck Oncol 2: 2-20.
- Akimoto T, Nonaka T, Kitamoto Y, Ishikawa H, Ninomiya H, et al. (2006) Radiation therapy for T2N0 laryngeal cancer: a retrospective analysis for the impact of concurrent chemotherapy on local control. Int J Radiat Oncol Biol Phys 64: 995-1001.
- Snthi T, Rajan KV (2016) Recurrence rate in post irradiated T1 and T2 supraglottic and glottic carcinoma of the larynx. Int J Sci Stud 3: 233-238.
- Pfister DG, Laurie SA, Weinstein GS, Mendenhall WM, Adelstein DJ, et al. (2006) American society of clinical oncology clinical practice guideline for the use of larynx-preservation strategies in the treatment of laryngeal cancer. J ClinOncol 24: 3693-3704.
- Nishimura G, Tsukuda M, Mikami Y, Matsuda H, Horiuchi C, et al. (2009) Efficacy of concurrent chemoradiotherapy for T1 and T2 laryngeal squamous cell carcinoma regarding organ preservation. Anticancer Res. 29: 661-666.
- Browman GP, Wong G, Hodson I, Sathya J, Russell R, et al. (1993) Influence of cigarette smoking on the efficacy of radiation therapy in head and neck cancer. N Engl J Med 328: 159-163.
- Chen AM, Chen LM, Vaughan A, Sreeraman R, Farwell DG, et al. (2011) Tobacco smoking during radiation therapy for head-and-neck cancer is associated with unfavorable outcome. Int J Radiat Oncol Biol Phys 79: 414-419.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences