Enlargement of ÃÆâÃâââ¬Ãâà âSHENOY NodeÃÆâÃâââ¬ÃâÃÂ: A Risk Factor for Temporary Recurrent Laryngeal Nerve Paralysis after Thyroid Surgery
Kapil Dev, Gurawalia J, Pandey A, Kumar S, Kurpad V and Shenoy AM2
DOI10.21767/2572-2107.1000015
Dev K1*, Gurawalia J1, Pandey A1, Kumar S1, Kurpad V1 and Shenoy AM2
1Department of Surgical Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India
2Department of Head and Neck Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India
- *Corresponding Author:
- Dev K
Room No 314, PG Hostel Men’s
Department of Surgical Oncology
Kidwai Memorial Institute of Oncology
Dr MH Marigowda Road, Bangalore, Karnataka, India.
Tel: +918026094000
E-mail: dr.kapil2010@gmail.com
Received date: September 26, 2016; Accepted date: October 17, 2016; Published date:October 24, 2016
Citation: Dev K, Gurawalia J, Pandey A, et al. Enlargement of “SHENOY Node”: A Risk Factor for Temporary Recurrent Laryngeal Nerve Paralysis after Thyroid Surgery. Head Neck Cancer Res. 2016, 1:3. doi: 10.21767/2572-2107.100015
Abstract
The incidence of temporary RLN paralysis is usually underestimated, which might be due to unabated or undetected vocal cord palsy or ignorance of mild hoarseness of voice by the patient himself or herself or by the physician. The rate of RLN paralysis with an overall range of 1% to 8.6%, with 1% to 5.1% as temporary paralysis, and 0 to 2.9% reported as permanent nerve paralysis. Enlarged lymph node located just anterior to the entry point of RLN into cricothyroid membrane, within a radius of 5 mm, might be a potent predictor of temporary nerve paralysis. A prospective observational study of patients who underwent thyroid surgery over a period of eighteen months, observing enlargement of lymph node in the area within a 5 mm radius of the entry point of RLN in cricothyroid membrane and correlated with incidence of temporary and permanent RLN paralysis, node was named as “SHENOY’s Node”. A total of 106 patients underwent thyroid surgery during the study period. The incidence of enlargement of lymph node was 10% and incidence of temporary RLN paralysis was 63%, twice to that in patients without an enlarged node. The relative risk of temporary and permanent RLN paralysis with enlarged node compared to without enlarging node was 2.01 (p<0.0001) and 3.03 (p=0.002), respectively. Patients with enlarged “SHENOY’s Node” is an additional risk factor of a higher rate of temporary RLN palsy during thyroid surgery.
Keywords
Thyroidectomy; Recurrent laryngeal nerve; Paralysis; Shenoy’s Node
Introduction
The clinically apparent recurrent laryngeal nerve (RLN) paralysis, temporary or permanent is an important issue for a thyroid surgeon [1,2]. Optimum exposure of the operative field with identification of anatomical landmarks are critical steps to evade inadvertent nerve injury. Recently, intraoperative nerve monitoring (IONM) to identify the nerves during thyroid surgery was shown to help lower the incidence of nerve injury, resulting better post-operative vocal cord outcomes [3]. The literature shows evidence of the rate of RLN paralysis with an overall range of 1% to 8.6%, with 1% to 5.1% as temporary paralysis, and 0 to 2.9% reported as permanent nerve paralysis [4-8].
The incidence of temporary RLN paralysis is usually underestimated, which might be due to unabated or undetected vocal cord palsy or ignorance of mild hoarseness of voice by the patient himself or herself or by the physician. There are several factors affecting the probability a the temporary RLN paralysis, such as large locally infiltrative extra-thyroidal disease, substernal extension of lesion, history of previous surgery or irradiation, surgery including central compartment lymph node dissection, presence of anatomical variation in nerve anatomy [2,9-13]. The incidence of enlarged para-tracheal lymph node either reactive or metastatic is reported as 23% to 60% in patients with suspicious malignancy or differentiated thyroid cancer [14].
The lymph node located posterior to the RLN has a strong relation with temporary RLN paralysis, although the incidence of metastasis to this node is half of that in nodes anterior to the RLN, and is reported as 17% versus 36%, respectively [14]. Enlarged lymph node located just anterior to the entry point of RLN into cricothyroid membrane, within a radius of 5 mm, might be a potent predictor of temporary nerve paralysis, which cannot be neglected during dissection to rule out metastasis. We here introduce a short study concerning to this specific node and its correlation with the incidence of temporary vocal cord paralysis, which has never been considered before.
Materials and Methods
From August, 2014 to April, 2016 a total number of One-hundred six patients with a diagnosis of thyroid swelling, including differentiated thyroid carcinoma (DTC), multinodular goitre (MNG), solitary thyroid nodule (intermediate or high risk), follicular neoplasm underwent thyroidectomy (lobectomy or total thyroidectomy) with or without neck lymph node dissection at our institute.
Preoperative evaluation
All patients were thoroughly examined, including clinical and systemic examination followed by a thyroid function test, ultrasonography neck, fine needle aspiration cytology of thyroid swelling and/ or cervical lymph, if clinical palpable or evident of imaging, MRI neck in case of DTC, serum tumor markers serum calcitonin and CEA were performed. All patients had normal mobility of both vocal cords confirmed with indirect Laryngoscope done in awake state. All relevant staging work-up was performed for all patients with DTC.
Intraoperative
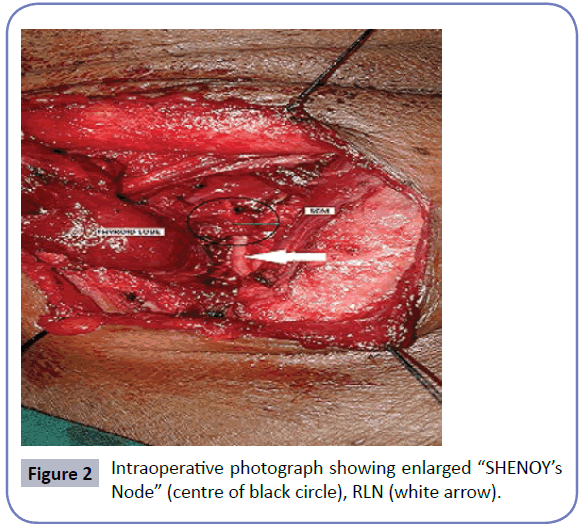
All patients after standard pre-anaesthetic assessment underwent thyroidectomy as described by Kocher, with trans-cervical transverse incision. All surgical steps were followed cautiously, except we approached from laterally between straps muscles and sternocleidomastoid muscle towards middle thyroid vein. We noted vigilantly all enlarged lymph nodes in para-tracheal region with special attention to the lymph node placed in the area of 5 mm radius from the RLN entry point into cricothyroid membrane which was named as “SHENOY’s Node” (Figure 1). In patients with enlargement of this node, nodal dissection in this area was done without the use of energy sources. Intra-operative frozen section was performed for this node to rule out metastasis and to avoid the inadvertent removal of the parathyroid gland.
Postoperative assessment
All patients were observed for any evidence of clinical hoarseness and underwent indirect Laryngoscope at 2-week and 6-week post-operatively to note the status of the vocal cords. Temporary RLN paralysis was defined as a decrease in vocal cord mobility with clinical evidence of hoarseness of voice at 2-week IDL, which improved at the time of the second examination at 6-week IDL.
Statistical analysis
We analyzed our data using SPSS 21.0 software from Microsoft. The correlation of variables with proportion was used chi-square test and ordinal variables were used mean and Mann-whitney test. The significant level was defined as value of p ≤ 0.05.
Results
Patients
A total number of one hundred six patients of thyroid swelling were included in our study, with a variety of diagnosis, including differentiated thyroid cancer (DTC) (n=70), multinodular goitre (n=17) and follicular neoplasm (n=19). DTC, papillary thyroid carcinoma (n=63) and medullary carcinoma (n=7) were also included. Majority of them were female (94%,89%). Median age at presentation was 41 years (range 19-72) (Table 1). All patients went through all preoperative assessment as described previous section.
| Characteristics | N=106 | |
|---|---|---|
| Gender | Male | 12 (11.30%) |
| Female | 94 (88.7%) | |
| Median age (Range) | 41 (19-72) Years | |
| Mean BMI (Kg/m2) | 21.4 (17.3-31.0) | |
| Hypo/Hyperthyroidism | 14 (13.20%) | |
| Previous thyroid surgery | 4 (3.7%) | |
| Median size of thyroid swelling (largest diameter on USG) (Range) | 3.2 (1.3-14) cm | |
| Diagnosis | DTC | 70 (66%) |
| MNG | 17 (16%) | |
| Follicular neoplasm | 19 (18%) | |
| Surgery | Hemi-thyroidectomy/ completion thyroidectomy | 31 (29.20%) |
| Total thyroidectomy without Neck dissection | 54 (50.90%) | |
| Total thyroidectomy with Neck dissection | 21 (19.90%) | |
Table 1: Descriptive parameters of whole study cases.
Intraoperative findings
35 patients had lymph node dissection done, the remainder of the patients underwent only thyroidectomy either total or hemithyroidectomy only. In eleven patients, we found the study node to be enlarged, with variation in size of range from 4 mm to 16 mm (median size 7 mm) in largest diameter (Figure 2). Median age, BMI, the median size of thyroid lesion, duration of surgery in patients with enlarged lymph node were not different from the rest of the patients (Table 2).
| Characteristics | Group A (n=11) | Group B (n=95) | p value | |
|---|---|---|---|---|
| Gender | Male | 1 (9.10%) | 11 (11.60%) | 0.9 |
| Female | 10 (90.90%) | 84 (88.40%) | ||
| Median age (Range) | 43 (22-72) Years | 44 (19-70) Years | 0.7 | |
| Mean BMI (Kg/m2) | 21.0 (17.3-30.4) | 21.2 (17.5-31.0) | 0.8 | |
| Hypo/Hyperthyroidism | 2 (18.20%) | 12 (12.60%) | 0.08 | |
| Previous thyroid surgery | 1 (9.10%) | 3 (3.15%) | 0.06 | |
| Median size of thyroid swelling (largest diameter on USG) (Range) | 4.0 (1.7-12) cm | 3.1 (1.3-14) cm | 0.06 | |
| Diagnosis | DTC | 7 (63.60%) | 63 (66.30%) | 0.09 |
| MNG | 2 (18.20%) | 15 (15.80%) | ||
| Follicular neoplasm | 2 (18.20%) | 17 (17.90%) | ||
| Surgery | Hemi-thyroidectomy/ completion thyroidectomy | 2 (18.20% | 29 (30.50%) | 0.2 |
| Total thyroidectomy without Neck dissection | 7 (63.60%) | 47 (49.50%) | ||
| Total thyroidectomy with Neck dissection | 2 (18.20%) | 19 (20%) | ||
Table 2: Characteristics of patients with enlargement "SHENOY’s Node" compared to patients without enlargement.
Post-operative short-term outcome
Forty-three (26.8%) patients were found to have evidence of RLN paralysis on clinical assessment at 2-weeks after surgery. Of these, fourteen patients had only clinical evidence of hoarseness of voice with only slight decrease in mobility of vocal cords, the rest of the cases were well evident on indirect laryngoscopy examination. In patients with enlarged study node, 9 out of 11 (81.8%) had RLN paralysis at 2-weeks after surgery and 2 out of 9 (18.2%) had permanent unilateral RLN paralysis at the end of 6-week follow up. Thus, rate of temporary RLN paralysis in our study group with enlarged study node was 63.6% and permanent RLN paralysis was 18.2%. One patient had partly improved at 18 months and another had persistence of RLN paralysis.
Patients without enlarging study node, 35 out of 95 (36.8%) had evidence of hoarseness and decrease of vocal cord mobility at 2-weeks post-operative visit. 30 out of 35 had recovered respect to clinical symptoms and vocal cord mobility as noted on IDL at 6-week. Five patients (5.3%) suffered from permanent RLN paralysis at the end of 6-week post operatively which was confirmed on IDL. Hence, the rate of temporary RLN paralysis in this group was 31.5% and permanent was 6%. The relative risk of temporary and permanent RLN paralysis with enlarged node compared to without enlarging node was 2.01 (p<0.0001) and 3.03 (p=0.002), respectively (Table 3).
| Temporary paralysis | Permanent paralysis | ||||||
|---|---|---|---|---|---|---|---|
| U/L | B/L | RR | U/L | B/l | Total | RR | |
| Group A (n=11) | 6 | 1 | 2.01 | 2 | 0 | 2 (18.2%) | 3.03 |
| Group B (n=95) | 25 | 5 | 4 | 1 | 5 (5.3%) | ||
| ÃÆÃÂÃâð2= 41.023; df=1; p<0.0001 | ÃÆÃÂÃâð2= 13.6345; df=1; p=0.0002 | ||||||
| U/L= Unilateral, B/L= Bilateral, RR= Relative risk |
Table 3: Risk of RLN paralysis with enlarged "SHENOY Node".
Discussions
Voice change is one of the most feared complication in patient undergoing thyroid surgery. The degree of RLN paralysis after thyroid cancer surgery is extremely variable. The impact on quality of life as well as clinical presentation of RLN paralysis mainly depends on its severity, unilateral versus bilateral nerve palsy, concomitant injury to superior laryngeal nerve, and baseline status of the vocal cords pre-operatively [15,16]. The range of the clinical severity of RLN palsy may extend from asymptomatic decrease movement of the vocal cords, hoarseness of voice, severe loss of voice, and aspiration to respiratory distress [10,15,16]. Thyroid surgery causing RLN palsy may prompt medico-legal litigations against the surgeon [1,2,17,18].
Both RLN and superior laryngeal nerve (SLN) are vulnerable to injury during thyroidectomy. Isolated SLN paralysis is rarely reported due to its mild consequences in the form of mild voice change, estimated at 3.7% [19]. The most severe complication due to the RLN injury is the occurrence of bilateral RLN paralysis leading to inability to abduct both vocal cords and severe respiratory distress, presents in 0.2% to 0.4% [19,20].
Recently, Sulica presented a review report of large number of patients (more than 28,000), and identified the rate of vocal cord paralysis as 1% to 8.6%. The proportion of temporary paralysis was much higher than permanent paralysis 1% to 5.1% versus 0 to 2.9%, respectively [4]. There are several technical issues that increase the risk of nerve injury. It may be due to unintentional stretching, thermal injury, entrapment by a ligature, excessive use of suction near the nerve, aggressive surgical dissection or ischemic injury [7,9,21]. Tumor factors include extra-thyroidal extension, substernal extension of enlarged thyroid, recurrent disease, enlarged central compartment lymph node. These factors were very well studied and are evident in the literature [2,6,10,13].
An important approach to avoid nerve injury is the careful dissection and identification of the nerve, although it is difficult with anatomical variations. During dissection, handling of tissue near the nerve usually results in transient ischemia, causing temporary nerve paralysis. The risk of nerve injury is highest near the entry point of nerve into the cricothyroid membrane [22,23].
Although with the use of modern techniques of magnification and intraoperative nerve monitoring helps surgeon to avoid the inadvertent injury to RLN, especially in case of variation in the expected course of the RLN. However, presence of extra-thyroidal extension of the disease in central compartment, enlarged lymph nodes could still be the reasons of high rate of RLN palsy. The routine central compartment lymph node dissection is mandatory in patients who have evidence of enlarged nodes intra-operatively with a pre-operative diagnosis of DTC on FNAC. Thus, this could be overcome by improving surgical technique only.
The incidence of enlarged lymph node either reactive or metastatic in the concerned area in the present study is not reported in the literature. We observed in our study over a short duration of eighteen months, the rate of study node enlargement as 10.3% (11 out of 106 patients). This is an important reason for the temporary vocal cord paralysis, and forms a high risk factor for unilateral temporary nerve palsy in comparison to patients who had no evidence of the study node enlargement. The relative risk of permanent RLN palsy is also higher in patients with enlarged study node but in view of very small number of patients, it is not significant to be presented as an evidence.
Although, both groups in our study were comparable regarding their pathological and intraoperative parameters. However, the significant discrepancy of rate of temporary RLN palsy between both the groups with relative risk of 2.01 (p<0.0001) and permanent with relative risk of 3.03 (p=0.002). This is a robust clinical evidence to increase awareness towards this specific node “SHENOY’s Node” in this region during thyroid surgery. Indeed, the rate of RLN paralysis is much more than reported in the literature due to the difference in the definition based on clinical symptoms and/or vocal cord abnormal mobility on indirect Laryngoscope and a small number of patients.
Based on this report, we recommend to put an extra effort during the dissection in the area near the RLN entry point to avoid this complication, and thus help to improve the quality of life postoperatively. Despite the short duration of study with a small number of patients, our results add new insight into the additional attention of the surgeon during thyroid surgery, highlighting its role in minimizing temporary RLN paralysis.
Conclusion
Although, nodal dissection in thyroid surgery, specifically around the entry point of RLN in cricothyroid membrane seemingly simple, is not. Thus, when we found enlargement of this node, we generally take an extra conscious at this particular step of surgery, if we fail, runs as an inexorable course towards postoperative morbidity. Patients with enlarged “SHENOY’s Node” is an additional risk factor of a higher rate of temporary RLN palsy during thyroid surgery.
Acknowledgements
We acknowledge to all patients to participate to study and the Department of Medical record and Epidemiology for the help to collect data and statistical analysis.
References
- Chiang FY, Lee KW, Chen HC (2010) Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg 34: 223-229.
- Dralle H, Sekulla C, Haerting J (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136: 1310-1322.
- Dionigi G, Frattini F (2013) Staged thyroidectomy: time to consider intraoperative neuromonitoring as standard of care. Thyroid 23: 906-908.
- Sulica L, Cultrara A, Blitzer A (2006) Vocal fold paralysis: causes, outcome and clinical aspects. In: Sulica L, Blitzer P (eds.), Vocal Fold Paralysis. New York, NY: Springer-Verlag, pp: 33-54.
- BarczyÃÆââ¬Â¦Ãâââ¬Å¾ski M, Konturek A, CichoÃÆââ¬Â¦Ãâââ¬Å¾ S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96: 240-246.
- Angelos P (2009) Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin N Am 89: 1157-1169.
- Chiang FY, Lu IC, Chen HC (2010) Anatomical variations of recurrent laryngeal nerve during thyroid surgery: how to identify and handle the variations with intraoperative neuromonitoring. Kaohsiung J Med Sci 26: 575-583.
- Sari S, Erbil Y, Sümer A (2010) Evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg 8: 474-478.
- Rulli F, Ambrogi V, Dionigi G (2014) Meta-analysis of recurrent laryngeal nerve injury in thyroid surgery with or without intraoperative nerve monitoring. Acta Otorhinolaryngol Ital 34: 223-229.
- Dralle H, Sekulla C, Lorenz K (2008) The German IONM Study Group: Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 32: 1358-1366.
- Horne SK, Gal TJ, Brennan JA (2007) Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol Head Neck Surg 136: 952-956.
- Calò PG, Pisano G, Medas F (2012) Risk factors in preoperative thyroid surgery for recurrent goitre. Our experience. G Chir 33: 335-338.
- Calò PG, Tatti A, Medas F (2012) Forgotten goiter. Our experience and a review of the literature. Ann Ital Chir 83: 487-490.
- Giordano D, Valcavi R, Thompson GB (2012) Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 22: 911-917.
- Bhattacharyya N, Fried MP (2002) Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg 128: 389-392.
- Chan WF, Lo CY (2006) Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 30: 806-812.
- Ready AR, Barnes AD (1994) Complications of thyroidectomy. Br J Surg 81: 1555-1556.
- Kern KA (1993) Medicolegal analysis of errors in diagnosis and treatment of surgical endocrine disease. Surgery 114: 1167-1173.
- Materazzi G, Dionigi G, Berti P (2007) One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1571 cases over a three-year period. Eur Surg Res 39: 182-188.
- Rosato L, Avenia N, Bernante P (2004) Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 28: 271-276.
- Chiang FY, Lu IC, Kuo WR (2008) The mechanism of recurrent laryngeal nerve injury during thyroid surgery-The application of intraoperative neuromonitoring. Surgery 143: 743-749.
- Hermann M, Alk G, Roka R (2002) Laryngeal recurrent nerve injury in surgery for benign thyroid diseases effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg 235: 261-268.
- Randolph GW (2003) Surgical anatomy of the recurrent laryngeal nerve. In: Randolph GW (ed.), Surgery of the Thyroid and Parathyroid Glands. 1st edn. Philadelphia, PA: Saunders, USA, pp: 300-342.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences