Minimally Invasive Approach in Surgical Treatment of Tumors of Maxilla
Dikarev A, Porhanov V, Kochergina E, Pavlov I, Kokaev K, Kutsenok M, Paramonova O and Savosin Y
DOI10.21767/2572-2107.100005
Dikarev A*, Porhanov V, Kochergina E, Pavlov I, Kokaev K, Kutsenok M, Paramonova O and Savosin Y
Head and Neck Surgery Department, Research Institute, Regional Clinical Hospital, 167, Maya St. Krasnodar, Krasnodar Region-350086, Russia
- *Corresponding Author:
- Dikarev A
Head and Neck Surgery Department, Research Institute
Regional Clinical Hospital, 167, Maya St. Krasnodar
Krasnodar Region-350086
Russia
Tel: 007(918)340-02-00
E-mail: asdikarev@gmail.com
Recieved date: Mar 10, 2016; Accepted date: Apr 02, 2016; Published date: Apr 04, 2016
Copyright: © 2016 Dikarev A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: By benign and malignant tumors of the maxillary sinus and maxilla there is frequently a need to perform a total maxillectomy. In this article we describe a transconjuctival-transoral approach, which can be evaluated in terms of esthetic result, complications, integrity of the important structures of the midface that provide physiological function and reduce the rehabilitation period.
Study design: We operated seven patients in the time between 2013-2014. Among them were four patients with malignant tumors with preoperative radiology treatment one patient with malignant tumor without preoperative radiology treatment and two patients with benign tumors. All these patients have no recurrence until now.
Methods: The surgical technique is performed in following steps: transconjunctival incision, exposure of the zygomatic bone, low orbital rim and orbital floor through precise dissection of the structures of the low eyelid, intraoral incision, traditional osteotomies with preserving the low orbital rim, lateral canthopexy, skin suturing.
Results: Reduction of the postoperative treatment period and complications, better esthetic results.
Conclusion: Transconjunctival-transoral approach benefits the conventional ones in fast rehabilitation, good esthetic results without facial scars and low eyelid malposition
Keywords
Malignant tumor; Benign tumor; Maxilla; Maxillary sinus; Atransconjunctival-transoral approach; Maxillectomy
Introduction
In the structure of morbidity the malignant tumors of maxillary sinus constitutes 0.2% to 1.4%. The most frequently affected structure in this group is maxilla. Specialty of the pathology is a generalized primary neglect of 80-85%. According to medical literature evidence [1-3] there are no distinct gender differences in the morbidity to be observed. Neoplastic process in the maxillary sinus mostly occurs in the patients’ group over 50 years old [4]. The most frequent pathology is squamous cell cancer.
In the majority of cases of benign and malignant tumors of the maxilla the predominant method of the treatment appears to be the surgical one [3]. The radicalism of the applied procedure ensures the best prognostic result [3]. One can determine the extent of the resection by the rate of expansion of the neoplastic process. In the cases where the maxillary sinus is involved, the therapy of choice is maxillectomy [4-7].
Lateral rhinotomy [8], Weber-Fergusson [2,9] approach and it’s modifications constitute the classical approach to the middle zone of facial skeleton [10,11]. The conventional methods mentioned above are transcutaneous with crossing of the superficial muscle-aponeurotic layer and the facial muscles. An outcome of the procedure appears to be the forming of scar tissue in the facial zones of high social significance. Furthermore, frequent complications could be asymmetry of the face, risk of the fistula and dehiscence of the incisional wound, scar tissue malposition on the inferior eyelid.
The report represents our experience on applying the surgical method of tumor resection in the middle zone of the face by means of combined transoral - transconjunctival approach. An extended incision in the face and a structural damage of the superficial muscular - aponeurotic system of the face will be thereby avoided, and the postoperative esthetic defects, among them the malposition of the inferior eyelid, will be minimized.
This minimal invasive approach reduces the period of rehabilitation for the patients’ group with tumors of the maxilla and zygomatic - orbital complex.
Aim of the study: the aim of this study is to present a modified method of the total maxillectomy that we are performing frequently in our clinic. Furthermore we attempt to prove that this method provides better esthetic results and reduces complications in comparison to the common ones. Lastly, the hospital could profit from the shorter rehabilitation period through the higher income and the lower clinical cost.
Materials and Methods
Patients
In our clinic in the period of 2013-2014 seven patients have been operated using this minimal invasive approach. Five of them have had malignant tumors of the maxilla (stage T3 - T4), four of which underwent adjuvant radiotherapy. The rest two patients have had benign tumors of the maxilla.
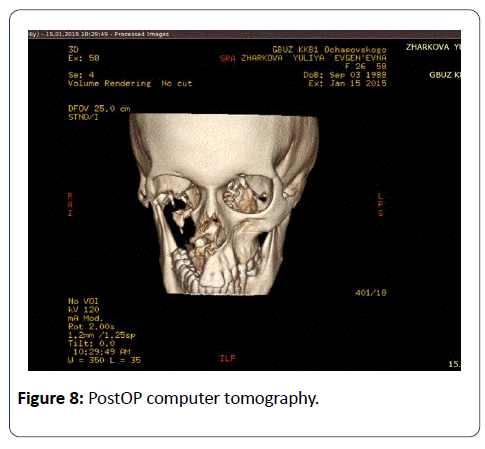
By all the cases CT scans with contrast were used for tumor staging, in accordance to the UICC - 2002 TNM Classification.
Surgical technique
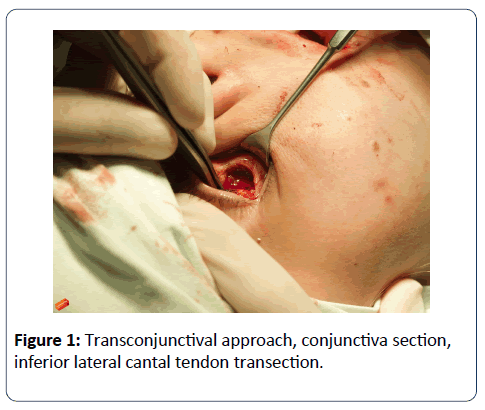
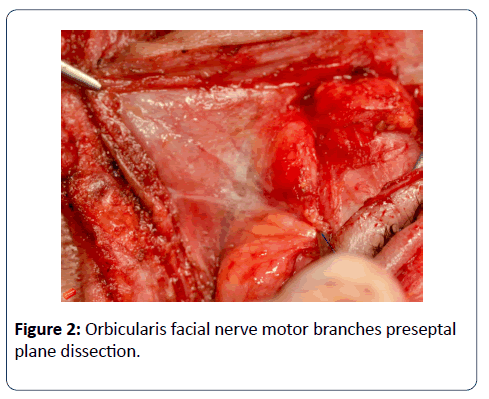
The operation was held under general anesthesia: We used the upper transconjunctival approach (Figure 1). The conjunctiva should be incised 2 mm from the edge of the lower tarsal plate. After finding the middle lamella we carry out a tissue dissection along the above mentioned structure leaving the orbicular muscle and orbital septum anatomically intact. We mobilize the orbicular muscle in the preseptal layer with preserving small branches of ramus zygomaticus of the facial nerve (Figure 2). On the inferior orbital rim the periosteum has to be incised and a subperiostal dissection of the orbital floor has to be carried out.
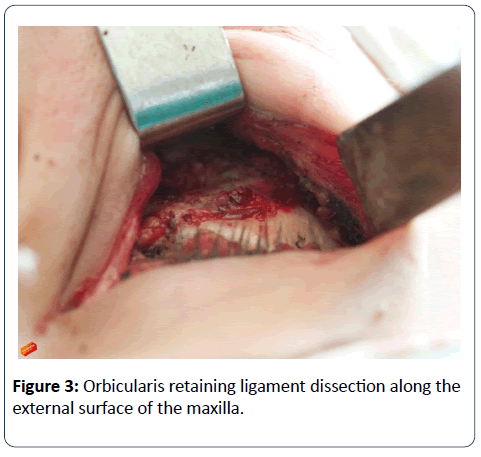
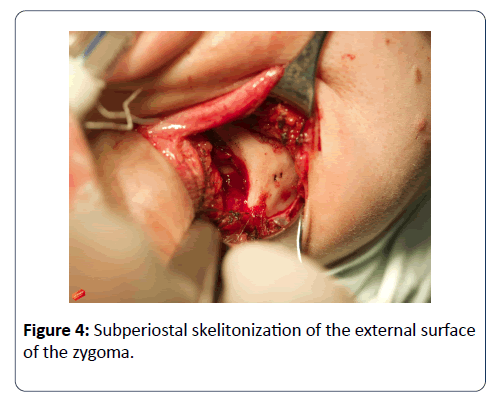
On the external surface of the maxilla downwards the lower orbital rim: we sharply cut off the orbicular retaining ligament (Figure 3), orbicular muscle, m. zygomaticus major and minor, m. levator anguli oris, m. levator labii superior. We cut the cantal ligament laterally and expose the surface of the zygomatic bone (Figure 4) and half of the zygomatic arch subperiostally, cutting off the ligament of the m. masseter throughout 3-4 mm. Afterwards we perform the resection of the tumor.
We incised oral mucosa along the mucobuccal fold of the maxilla from the maxillary tuber to the level of the first incisor and then downwards. The anterior surface of the maxilla is dissected subperiostally. Further, the incision is made between central incisors along the hard palate vertically till the level of the soft palate and then horizontally lengthwise till the border of the hard palate in the direction of the maxillary tuber.
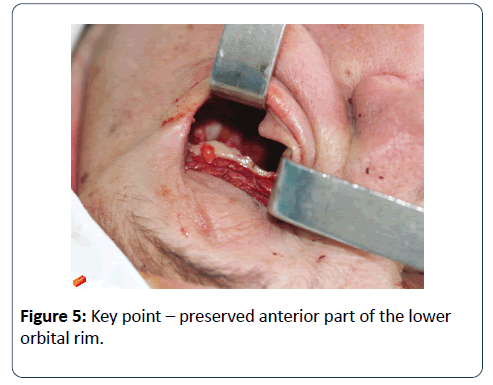
We made osteotomies along the nasal process of the maxilla, lacrimal bone, zygomatic bone and the middle line of the hard palate. According to the indications, it is possible to preserve the lower orbital rim in the form of the bridge from the body of the zygomatic bone to the nasal bone (Figure 5). As the last step we perform the detachment of the maxillary tuber from the pterygoid process of the sphenoid bone.
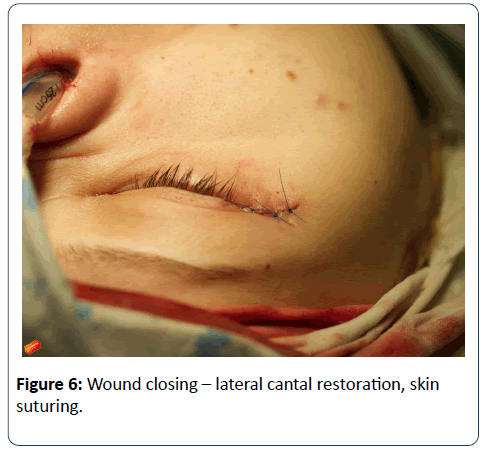
After the removal of the resected specimen (Figure 6) and antiseptic irrigation of the resection zone we perfom the standard lower lateral canthopexia. The fixation has to be carried out to the remained lateral part of the cantal ligament or to the lateral orbital rim itself with drill holes.
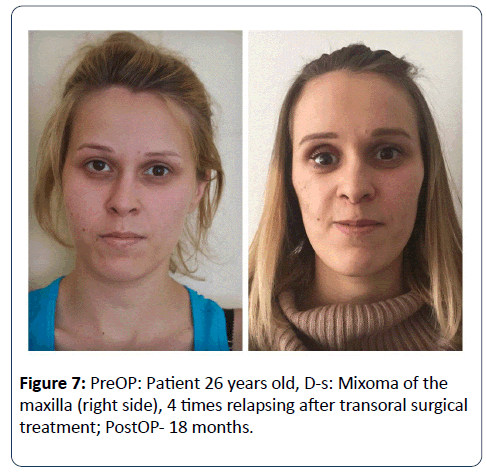
We sutured skin incision of the lateral eye angle area with interrupted sutures Prolene Nº 6 (Figure 7), removed on the 3th day. We have placed mattress suture Monocryl Nº 6 on conjunctiva. We used Levomekol wound salve and gas packing. In the intra- and postoperative period we prescribed broad - spectrum antibiotics for all the patients.
The postoperative period passed according to the standard without any complications. All the patients left the clinic on the 4th day. By now all the patients are observed without relapsing (Figure 8).
Results
The suggested method was used in 7 patients in general: among them were four patients with malignant tumors with preoperative radiology treatment one patient with malignant tumor without preoperative radiology treatment and two patients with benign tumors. Herewith we have achieved a reduction of postoperative treatment period in comparison with patients, by whom were performed equivalent tumor resection by means of classical transcutaneous approaches. All patients had to stay in the hospital for an average of 4 days, the sutures could be removed after only 7 days.
Discussion
Traditional approaches as lateral rhinotomy and Weber - Fergusson approach and its modifications are normally used for the total and subtotal maxillectomy by malignant and benign tumors of the maxilla [12] and maxillary sinus. Those approaches provide good visualization, but most of the patients receive adjuvant radiortherapy, that can cause fistulae and dehiscence of the wound in the postoperative period. Furthermore, traditional approaches cause extended facial scars.
Atransconjunctival - transoral approach avoides broad transfacial incisions and gives a surgeon a sufficient visualization of the field with a possibility to perform a precise resection according to the standard of radicalism with intraoperative appropriate control of the margins. The reduction of complications and recovering period compensates the difficulty of the approach. The outcome is followed by good esthetic result without lower eye lid and eye globe malposition.
The major indication of the described method seems to be the unilateral malignant tumors of the maxillary bone and sinus. This process should not be used on the other hand by bilateral or unilateral tumors where the ethmoid bone, the nasal cavity and the skin are involved.
As far as we know this is the first report about such transconjunctival - transoral approach with preserving the lower orbital rim as a supporting structure of the eye globe after the maxillectomy in comparison to standard approaches. The most important limitation of this study was the small sample of patients, because of the rarity of the pathology in this specific localization. A second limitation is the short follow - up because the approach performed and described is new.
Conclusion
In all cases we performed surgical treatment according to the principles of radicalism. That was proved both by intraoperative and routine pathohistological examination. We succeeded in excluding incisions on the face, as well as avoiding the structural damaging of the superficial muscular-aponeurotic system and the mimic muscles. We also managed to minimize the esthetic defects.
The rehabilitation period of the patients with tumors of facial skeleton in the middle zone of the face, maxilla and zygomatic - orbital complex was reduced. The risks of the inferior eyelid malposition were minimized.
By now all of the patients are observed without relapse and undergone prosthetic rehabilitation [13].
Conflict of Interest Statement
The authors, whose names are listed, certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Patel SG, Singh B, Polluri A, Bridger PG, Cantu G, et al. (2003) Craniofacial surgery for malignant skull base tumors: report of an international collaborative study. Cancer 98: 1179-1187.
- Atlas of Head and Neck Surgery (2001) Otolaryngology. LLW,pp: 26-32.
- Shah J (2003) Head and Neck Surgery and Oncology. (3rd edn) Mosby,pp: 57-93.
- Sisson GA Sr, Toriumi DM, Atiyah RA (1989) Paranasal sinus malignancy: a comprehensive update. Laryngoscope 99: 143-150.
- Liu Z, Yu H, Wang D, Wang J, Sun X, et al. (2013) Combined transoral and endoscopic approach for total maxillectomy: a pioneering report. J NeurolSurg B Skull Base 74: 160-165.
- Ami LP, Chad AZ (2010) Total Maxillectomy. Operative Tech in Otolyringo 21: 166-170.
- Rivera-Serrano CM, Terre-Falcon R, Duvvuri U (2011) Combined approach for extensive maxillectomy: technique and cadaveric dissection. Am J Otolaryngol 32: 417-421.
- Vural E, Hanna E (2000) Extended lateral rhinotomy incision for total maxillectomy. Otolaryngol Head Neck Surg 123: 512-513.
- Ali AH, Benay Y (2013)Right hemi-maxillectomy via Weber Ferguson approach for the management of squamous cell carcinoma of the maxilla and paranasal sinuses. Oral Oncology. World Congress of the International Academy of Oral Oncology (IAOO) 49:1.
- deFries HO, Deeb ZE, Hudkins CP (1988) A transfacial approach to the nasal-paranasal cavities and anterior skull base. Arch Otolaryngol Head Neck Surg 114: 766-769.
- Tiwari RM (2001) Transmandibular approach to total maxillectomy. Indian J Otolaryngol Head Neck Surg 53: 187-189.
- Soni R, Jindal S, Singh BP, Mittal N, Chaturvedi TP, et al. (2011) Oral rehabilitation of a patient with sub-total maxillectomy. Contemp Clin Dent 2: 63-65.
- Kawase-Koga Y, Saijo H, Hoshi K, Takato T, Mori Y (2014) Surgical management of odontogenicmyxoma: a case report and review of the literature. BMC Res Notes 7: 214.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences