How to Treat Sweat Gland Adenocarcinoma of the Eyelid: Case Report
Hiroyuki Maeda
DOI10.21767/2572-2107.100017
Hiroyuki Maeda*
Department of Otorhinolaryngology, Head and Neck Surgery, Graduate School of Medicine, University of the Ryukyus, Nishihara-cho, Okinawa, Japan
- *Corresponding Author:
- Hiroyuki M
Department of Otorhinolaryngology
Head and Neck Surgery, Graduate
school of Medicine, University of the Ryukyus
Nishihara-cho, Okinawa, Japan
Tel: 098-895-1183
Fax: 098-895-1428
E-mail: maeidahiroyuki@yahoo.co.jp
Received Date: 28 June 2017 Accepted Date: 01 July 2017 Published Date: 09 July 2017
Citation: Maeda H. How to Treat Sweat Gland Adenocarcinoma of the Eyelid: Case Report. Head Neck Cancer Res. 2017, Vol.2 No.1:2. doi:10.21767/2572-2107.100017
Copyright: ©2017 Maeda H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: It is thought that apocrine gland carcinoma in the eyelid is rare and its prognosis is very poor. To achieve a curative treatment, we must remove the tumour with surrounding normal tissue, such as orbital contents or the skin of the face, in which case the loss of physiologic lacrimal function and facial cosmesis are serious concerns.
Methods: A case presentation, treatment, and review of the literature and discussed.
Results: Patient was a 54-year-old male. The tumour at the right inferior eyelid extended to the upper eyelid via the medial can thus, infraorbital fat tissue and medial rectus muscle. We performed a curative operation. The tumor was removed completely, along with the medial side of the eyelids, orbital contents and the right maxillary bone.
Conclusions: We performed the treatment for adenocarcinoma of the eyelid. As a result, we could obtain patient’s and his families’ satisfaction.
Keywords
Sweat gland; Apocrine gland; Adenocarcinoma; Lacrimal drainage system; Eyelid
Introduction
In the malignant tumors of the eyelid and orbital fossa, adenocarcinoma is also found relatively often [1]. Almost all sebaceous gland carcinomas are adenocarcinomas [2]. Sweat gland carcinoma, which arises from apocrine glands of the eyelid cilia, is very rare [3]. However, local recurrence and cervical lymph nodes and distant metastases are common in apocrine gland carcinoma and prognosis is generally very poor [4]. We treated a patient with apocrine gland carcinoma that arose from the inferior eyelid. We think that the tumor was derived from Moll’s gland.
In this manuscript, we report how we tried to preserve curativity, facial cosmesis, and function of the nasolacrimal gland.
Case report: Patient: 54-year-old male; C.C: Right under eyelid swelling; P.H: W.N.L; F.H: W.N.L.
Presence: The patient had noticed his right inferior eyelid swelling. When he visited the eye clinic, an intraorbital tumour was identified. A small part of the tumour was resected and histologic examination identified the tumour as an adenocarcinoma. The patient was sent to our institute for examination and treatment.
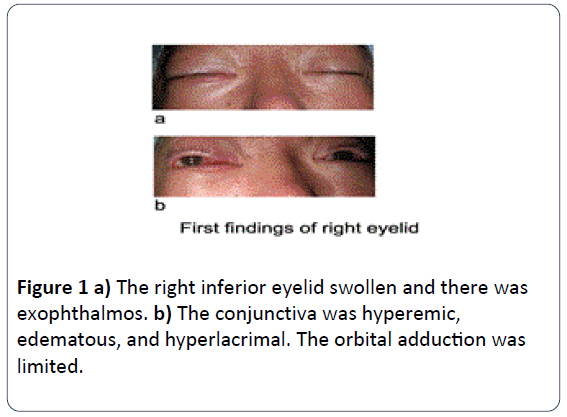
Presentation: The right inferior eyelid was remarkably swollen and the tumour invaded the intraorbital fossa. The conjunctiva was hyperemic, edematous, and hyperlacrimal. There was right exophthalmos, and orbital adduction was limited. The skin around the right eyelid was neither red nor swollen (Figure 1a and 1b). Moreover, no cervical lymphadenopathy was evident.
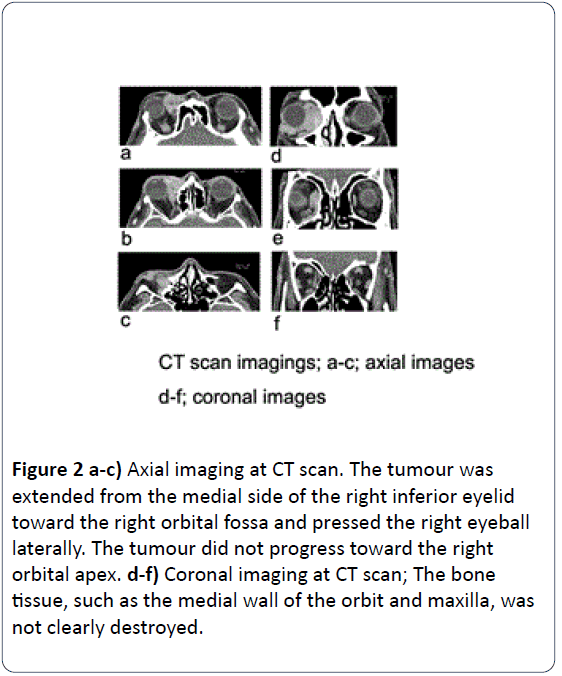
Imaging findings: On CT imaging, the tumour was strongly radiopaque and extended from the medial side of the right inferior eyelid toward the right orbital fossa and pressed the right eyeball laterally. The tumour did not progress toward the right orbital apex. The bone tissue, such as the medial wall of the orbit and maxilla, was not clearly destroyed. However, the tumour invaded inside the right nasal cavity and maxillary sinus through a rumen of the nasolacrimal duct (Figure 2a-2f).
Figure 2: a-c) Axial imaging at CT scan. The tumour was extended from the medial side of the right inferior eyelid toward the right orbital fossa and pressed the right eyeball laterally. The tumour did not progress toward the right orbital apex. d-f) Coronal imaging at CT scan; The bone tissue, such as the medial wall of the orbit and maxilla, was not clearly destroyed.
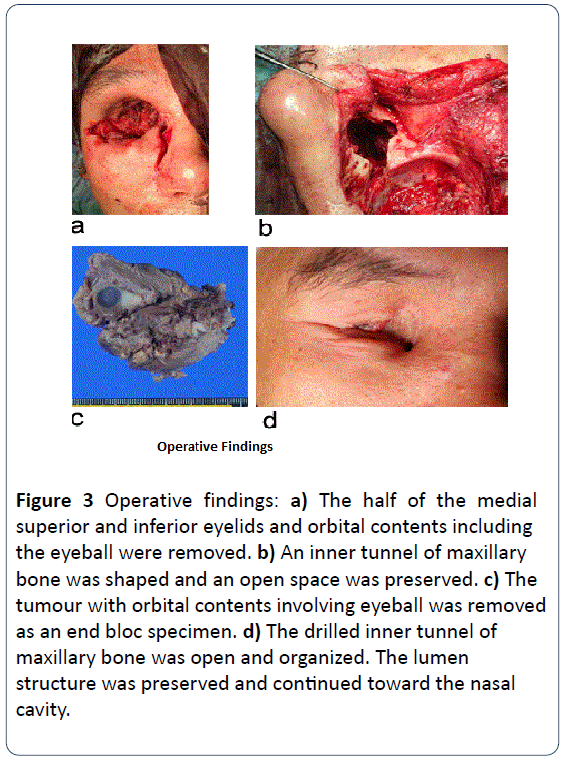
Operative findings: At first, we removed half of the medial superior and inferior eyelids and orbital contents, including the eyeball, as an end bloc specimen (Figure 3a). Next, we incised and opened the skin at the nasal dorsum, from the medial canthus to the nasal wing. We turned up the skin flaps and found the lacrimal sac, which was removed with the maxillary process. Then, the right nasolacrimal duct was exposed. We resected this duct inside the nasal cavity as we explored whether or not the duct was invaded by the tumour.
As a result, the inner mucous membrane of the maxillary sinus was removed, along with the concha nucae inferior. An inner tunnel of maxillary bone was shaped and an open space was preserved (Figure 3b). At last, the lower surface of the orbit was covered by a full-thickness skin graft taken from the medial thigh. No primary reconstruction using a skin flap or scapula was performed at the time.
Figure 3: Operative findings: a) The half of the medial superior and inferior eyelids and orbital contents including the eyeball were removed. b) An inner tunnel of maxillary bone was shaped and an open space was preserved. c) The tumour with orbital contents involving eyeball was removed as an end bloc specimen. d) The drilled inner tunnel of maxillary bone was open and organized. The lumen structure was preserved and continued toward the nasal cavity.
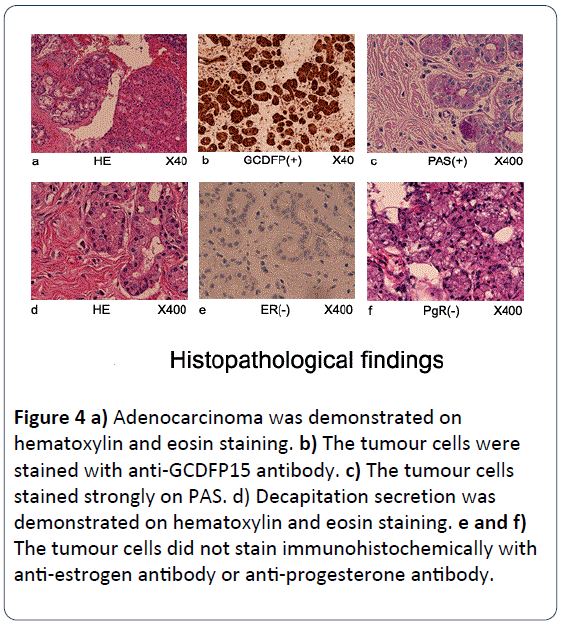
Pathological findings: c) We explored the hard mass along the medial side of the eyeball and circumstantially removed normal nasolacrimal tissue in the specimen d) Decapitation secretion was demonstrated on haematoxylin and eosin staining. The tumour cells were stained immunohistochemically with anti-GCDFP15 (Gross Cystic Disease Fluid Protein 15) antibody (Figure 4b) The tumour cells stained strongly on PAS but did not stain immunohistochemically with anti-estrogen antibody or antiprogesterone antibody (Figure 4c, 4e and 4f).
Figure 4: a) Adenocarcinoma was demonstrated on hematoxylin and eosin staining. b) The tumour cells were stained with anti-GCDFP15 antibody. c) The tumour cells stained strongly on PAS. d) Decapitation secretion was demonstrated on hematoxylin and eosin staining. e and f) The tumour cells did not stain immunohistochemically with anti-estrogen antibody or anti-progesterone antibody.
Final diagnosis: adenocarcinoma in the apocrine gland and eyelid.
Prognosis: One year after operation, the raw surface of the orbital floor was astringed and covered by new fibrous tissue. The postoperative space of the orbit was almost filled with connective tissue. Because the medial sides of the superior and inferior eyelids were absent, the function of the eyelids had almost been lost. The patient's eyelids were usually closed. However, incongruity of the face was not remarkable when wearing spectacles. Moreover, the drilled inner tunnel of maxillary bone was open and organized. The lumen structure was preserved and continued toward the nasal cavity (Figure 3d).
Discussion
Most tumours arising from the eyelids are basal cell carcinomas, squamous cell carcinomas, or keratoacanthomas [2]. Rarely, a sebaceous gland tumour in an epidermal appendage is reported [3] (Table 1). The sweat gland tumour arising from the eyelids such as we experienced is even more rare [4]. The sweat gland tumours are distributed eccrine gland and apocrine gland tumours. Usually, the eccrine glands secrete serous fluid, while the apocrine glands secrete viscous fluid such as mucin [2,4,5]. Moll’s gland is the proper term for the apocrine glands of the eyelid. Because the apocrine glands exist mainly at the axilla, anus, genitalia, external ear meatus and eyelid, most of the apocrine gland tumours occur in these locations. This local frequency of occurrence is important to consider in diagnosis and treatment [6]. Another criterion for diagnosis is pathological findings. Hyper eosinophilic matrix inside the tumour cells and decapitation secretion are characteristic findings for apocrine glands. Decapitation secretion is an interesting secretion style. The secretory process of secretory cells leads into the secretory duct and produces a hyper viscous liquid. Furthermore, positive PAS staining is found inside the tumour cells and rumen because mucous fluid secreted from the apocrine glands involves a large quantity of mucin [7]. Moreover, apocrine gland tumours stain with anti-GCDFP15 antibody, which is a specific marker for apocrine gland and breast cancer [7]. In addition, we made sure that these tumour cells did not stain with anti-estrogen and anti-progesterone antibodies, to avoid mismanaging such a tissue as a metastatic mammary carcinoma in our institute. As mentioned above, the apocrine gland tumour is diagnosed from pathological findings and the existence of apocrine glands in the region from which the tumour arises. Our patient’s tumour fulfilled all these conditions.
| Basal cell carcinoma |
|---|
| Basal cell nevus syndrome |
| Squamous cell carcinoma |
| Keratoacanthoma |
| Adenocarcinoma |
| Sebaceous gland carcinoma arising from the Zeis gl. the Meibomian gl. |
| Sweat gland carcinoma arising from the Eccrine gl. the Apocrine gl. (Moll’s gl.) |
| Lymphoma |
| Malignant melanoma |
| Merkel cell tumor |
| Rhabdomyosarcoma |
| Metastatic eyelid carcinoma |
Table 1: The category of the malignant tumour arising eyelid.
The tumour extended around the various tissues such as eyeball, orbital apex, skull base, the nasal and paranasal cavities, and skin of the face with direct invasion [8]. In general, it is thought that the invasion is slow. However, the tumour is prone to metastasize to parotid glands, cervical lymph nodes or distant organs such as lung and bone [1].
The efficacy of irradiation and chemotherapy is generally considered poor for this type of carcinoma, and only surgical treatment can offer the hope of a cure. An important issue for dissection of a tumour rests across two points. One is the dissection area of the primary tumour and reconstructive methods of the face. The other is whether or not the parotid gland and neck lymph nodes without metastasis of the tumour are dissected [9]. Needless to say, we must aim for cure when operating. Here, we had to remove the orbital contents and incise the skin of the face, including the eyelid, with as wide a margin as possible. However, facial cosmesis problems arise. In case of removal of orbital contents, we must prepare the eye socket at the orbital floor for a prosthesis. Moreover, everything possible must be done to preserve the physiological function of the lacrimal gland and nasolacrimal duct, and if we can preserve the eyeball, we must preserve the function of the eyelid to protect the eyeball from drying out. Similarly, if the lacrimal organs must be resected, reconstruction of those organs will be needed [10]. In our case, the orbital contents were completely removed, along with the affected part of the eyelid to prevent recurrence of the tumour. Then, a fullthickness skin graft, derived from the skin of the thigh, was performed on the raw surface to be able to find potential recurrence of the tumour easily. For this reason, we do not usually reconstruct using free flaps in our institute.
However complete our facial reconstruction, the recipient site looks heterogenous, and patients are not sure to be satisfied. In such cases, we think that the patient will be more comfortable wearing an epitase on the effected side of the face rather than reconstruction of the face using free flaps. In such a case, the raw surface in the orbital floor must be covered by skin graft, as in our case. Thereafter, we must choose the method and timing of the reconstruction using local or free flap as a secondary reconstruction to preserve cosmetic elements [11]. In the case that orbital contents are removed, a pool of lacrimal or seborrheic discharge is occasionally found. To drain away such discharge, we scooped out the facial bone from the maxillary process to the concha nucae inferior, inside the nasal cavity, after removing the nasolacrimal duct and making a new duct [12]. Accordingly, it was thought that pooled discharge on the orbital fossa was induced and drained away toward the nasal cavity. As a result, a recipient bed of the orbital fossa epithelialized perfectly, and the patient was satisfied with the cosmetic change of the face by wearing the epitase. Moreover, the drainage duct from the orbital fossa to the nasal cavity was opened definitively. It was thought this duct accomplished the drainage in a functional aspect.
On the other hand, another problem remained: whether or not to remove the parotid gland or cervical lymph nodes without metastases of the tumour. In other words, whether or not cervical lymph node dissection with a parotid gland must be performed at the time of the primary operation. Alternatively, we may perform an additional operation if the tumour recurs [9]
There is no specific evidence on whether cervical lymph node dissection should be performed unilaterally or bilaterally [13]. In the present case, we aimed to preserve the parotid gland and cervical organs on the assumption that the patient would be closely observed for severity after primary operation.
Conclusion
We reported concrete surgical treatment in the case of apocrine gland carcinoma of the eyelid (Moll’s gland). Surgical resection is the most important method for the patient to achieve a lasting cure. However, it was thought that we must choose appropriate surgical methods at the time of primary operation to satisfy the patient with curative treatment, retained cosmetics, and maintained function of facial organs.
References
- Warkel RL (1984) Selected apocrine neoplasms. J Cutan Pathol 11: 437-449.
- Latorre A, Alghothani L, Lambert D, Jatana KR, Sara Peters C, et al. (2012) Mucin-producing Malignant Tumor of Lower Eyelid Presenting in a 14-year-old Patient. J Clin Aesthet Dermatol 5: 44-47.
- Deo SV, Shukla NK, Singh M, Jha D, Khanna P, et al. (2012) Locally advanced sebaceous cell carcinoma (T3) of eyelid: incidence and pattern of nodal metastases and combined modality management approach. Orbit 31: 150-154.
- Inozume T, Kawasaki T, Harada K,Tanaka K, Kavamura T, et al. (2012) A Case of endocrine mucin-producing sweat gland carcinoma. Pathol Int 62: 344-346.
- Zhang Q, Wojno TH, Fitch SD, Grossniklaus HE (2010) Mucinous eccrine adenocarcinoma of the eyelid: report of 6 cases. Can J Ophthalmol 45: 76-78.
- Kipkie GF, Haust MD (1958) Carcinoma of apocrine glands. Arch Dermatol 78: 440-445.
- Paties C, Taccagni GL, Papotti M, Valente G, Zangrandi A, et al. (1993) Apocrine carcinoma of the skin; a clinicopathologic, immunocytochemical, and ultrastructural study. Cancer 71: 375-381.
- Akhtar I, Ispas CL, Flowers R,Siddiqi A,Young L, et al. (2009) Ductopapillary apocrine carcinoma of the eyelid metastatic to the parotid gland: report of a case diagnosed by fine-needle aspiration biopsy. Diagn Cytopathol 37: 91-95.
- Chieko Y, Norikazu Y, Motoyasu H, Tomoko S, Tetsuo H (2002) A Case of Apocrine Carcinoma of the Eyelid with Parotid Gland Lymph Node Metastasis. Pract Otol 95: 1045-1048.
- Wilson KF, Ward PD, Spector ME, Marentette LJ (2011) Orbitocranial approach for treatment of adenoid cyctic carcinoma of the lacrimal gland. Ann Otol Rhinol Laryngol 120: 397-400.
- Kobayashi K, Ishikawa H, Murakami R, Kinoshita N, Tokunaga K (2008) Total lower eyelid reconstruction with a prefabricated flap using auricular cartilage. J Craniomaxillofac Surg 36: 59-65.
- Heindl LM, Junemann AG, Kruse FE, Holbach LM (2010) Tumors of lacrimal drainage system. Orbit 29: 298-306.
- Jackson GL, Ballantyne AJ (1981) Role of parotidectomy for skin cancer of the head and neck. Am J Surg 142: 464-469.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences